آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
Introduction
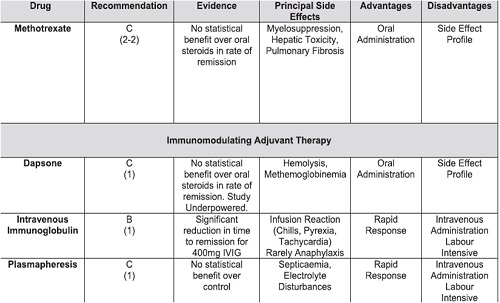
Treatment modalities in pemphigus vulgaris (PV) and pemphigus foliaceus (PF) are many and varied, although level 1 evidence supporting their use is limited.
To date, only 2 systematic reviews exist to support the use of different treatment modalities to control this group of conditions.
Overall, within the literature, the quality of trials comparing treatment modalities is poor. Cohort sizes are small, methodologies are varied, and standardized outcome measurements are lacking.
There is a paucity of high-quality, randomized, double-blind, control clinical trials to accurately assess interventions in pemphigus.
Although the number of high-quality trials does slowly increase with time, the evidence currently available does allow us to evaluate the efficacy of the more common modalities, such as glucocorticoids, immunomodulating,and antiinflammatory agents.
The authors aim to present a comprehensive view of the level 1 evidence that exists for common treatment modalities used in PV and PF.
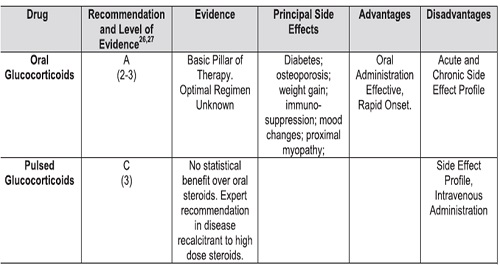
SYSTEMIC GLUCOCORTICOIDS
Steroids have been used as the baseline treatment and cornerstone of pemphigus management since the 1950s.
Although the efficacy of steroids as compared with no intervention is undisputed, the optimal regimen is still unclear.
Ratnam’s randomized controlled trial (RCT) comparing low-dosage (45–60 mg/d) with high-dosage (120– 180 mg/d) prednisone did not demonstrate a difference in any outcome, including the time to disease control and relapse rate.
All patients achieved remission; however, with only 22 participants, it was inadequately powered. Most expert opinions suggest the initial use of 1 mg/kg/d corticosteroids.
The long-term morbidity of glucocorticoids is probably reflected more by the cumulative dose rather than the starting dose, which emphasizes the role of appropriate dose-reduction of steroids when disease control is achieved.
Continuous Versus Pulsed Glucocorticoid Regimens
An RCT of 20 participants was published evaluating the efficacy of adjuvant pulsed oral dexamethasone (300 mg over 3 days monthly) in patients concurrently treated with prednisolone and azathioprine.
There was no difference demonstrated in the time to remission (averaging 173 days for the intervention cohort and 176 days for the placebo control cohort), rate of remission or duration of remission.
Moreover, the pulsed steroid group experienced considerable adverse events related to the high-dosage steroid.
This regimen involved extremely high monthly oral steroid dosages continued for several months after disease control had been achieved, and did not include patients with severe refractory disease for whom pulsed steroids are most likely to be of benefit.
These 2 studies both indicate the role for an individual approach to steroid dosage, with dynamic alteration of the dosage according to disease severity and patient response.
Although the early case series of pulsed corticosteroids appeared promising, evidence from controlled trials shows at pulsed corticosteroids confer no additional benefit and may be associated with more severe side effects. However, patients in these controlled trials were predominantly newly diagnosed, and whether pulsed corticosteroid therapy is beneficial for a subset of patients with severe refractory disease is not clear.
SYSTEMIC NONSTEROIDAL IMMUNOMODULATING THERAPIES
Systemic nonsteroidal immunomodulating therapies are typically slow-acting treatments used as maintenance therapies in pemphigus.
When combined with systemic glucocorticoids, they often promote disease control while having the added benefit of exerting a steroid-sparing effect caused by the reduction in the amount of glucocorticoid that would have previously been needed to achieve the same level of control.
Although the clinical significance of this steroid-sparing effect is still debated in the dermatologic community, the steroid-sparing benefit demonstrated in oncological and transplant medicine is likely to be applicable to pemphigus.
Chams-Davatchi conducted a landmark multiarm
RCT into the steroid-sparing role of adjuvants, comparing prednisolone alone with 3 adjuvant agents: mycophenolate, azathioprine, and pulsed cyclophosphamide.
he study demonstrated a significant decrease in the total dose of glucocorticoids when prednisolone was combined with a cytotoxic agent using analysis of variance.
The average cumulative prednisolone dosages over 12 months were as follows: prednisolone alone 11,631 mg, azathioprine 7712 mg, mycophenolate 9798 mg, and cyclophosphamide 8286 mg.
No differences were detected in clinical end points, including time to partial response, complete response, and treatment failure.
Immunosuppressive Therapies Azathioprine
Azathioprine is a purine synthesis inhibitor originally developed for use in organ transplantation.
Azathioprine has been evaluated in 3 RCTs, including comparisons with glucocorticoids alone (prednisolone),cyclophosphamide,and mycophenolate.
Chams-Davatchi’s study demonstrated a steroid-sparing benefit of azathioprine compared with prednisolone alone (P =.047), although no difference was noted in clinical end points.
In a meta-analysis of 2 studies including 92 patients, Martin and colleagues found a steroid sparing role for azathioprine compared with mycophenolate (2074 mg prednisone saved, 95% confidence interval.
In contrast, however, mycophenolate showed superior disease control.
Of note, this result was obtained with inclusion of a participant who withdrew after randomization, but before commencement of therapy, and results of the per-protocol analysis performed by the investigators were inconclusive.
In light of these disparate findings, there is currently insufficient evidence to draw a conclusion on the relative efficacy of azathioprine compared with mycophenolate.
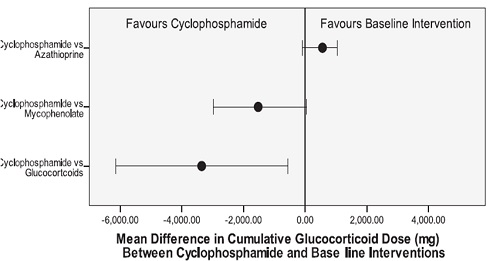
In their meta-analysis, Martin and colleagues found a superior steroid-sparing role for cyclophosphamide compared with azathioprine.
However, the statistical analysis conducted by the investigators, which accounted for comparison of multiple groups, found no significant difference .
There was weak evidence of a benefit for azathioprine over cyclophosphamide in disease control.
however, this is based on a study with small patient numbers. The evidence comparing azathioprine with cyclophosphamide is inconclusive.
At this stage, selection is advised on an individual basis regarding patient age, fertility, and comorbidities.
Cyclophosphamide
Cyclophosphamide is an alkylating agent that selectively inhibits lymphopoietic cells while sparing hematopoietic cells. It has been shown to be useful in a wide variety of autoimmune conditions by inhibiting cyclical production of antibody-producing B lymphocytes.
Martin’s systematic review identified studies that included comparisons of cyclophosphamide against glucocorticoids, azathioprine, cyclosporine, and mycophenolate.
There was a significant steroid sparing effect when combined as compared with prednisone alone.
The steroid-sparing effect of cyclophosphamide was found to be greater than that of mycophenolate mofetil and lesser than that of azathioprine as shown in Fig. 1. It must be noted, however, that reduction in cumulative steroid dose is a surrogate outcome.
Cyclophosphamide can be administered intravenously
(IV) or orally. A study of 28 patients was conducted comparing pulsed intravenous dexamethasone-cyclophosphamide plus daily oral cyclophosphamide with pulsed IV cyclophosphamide and daily oral prednisolone.
This study demonstrated earlier remission in the pulsed cyclophosphamide/oral prednisolone group (mean 7.3 weeks vs 3.2 weeks, P = .02); however, no difference was demonstrated in overall remission or relapse.
When comparing Cyclophosphamide with other
immunosuppressive medications, no significant difference was seen in any clinical outcomes when comparing cyclophosphamide and mycophenolate.
No difference in any outcome,including time to disease control or relapse, was found when cyclophosphamide was compared with cyclosporine in a small study of 18 participants.
A major drawback to the use of cyclophosphamide is its safety profile, which is discussed later.
Mycophenolate
Mycophenolate has been evaluated in 3 RCTs, including comparisons with glucocorticoids, azathioprine,and cyclophosphamide.
Beissert’s recent article comparing mycophenolate with placebo in 96 patients showed no statistically significant difference between the rates of response of glucocorticoids and mycophenolate and glucocorticoids plus placebo.
However, the addition of mycophenolate mofetil had a significant impact in hastening the average time to disease control (31.3 weeks in placebo vs 24.1 weeks in mycophenolate) and in delaying the average time to relapse (relapse rate at 24 weeks was 44.5% in the placebo group vs 21.8% in the mycophenolate group .
Beissert and colleagues also found a significant decrease in the total amount of glucocorticoid required from week 12 to week 52 in the mycophenolate group when compared with the placebo group , although no difference was observed in the total steroid dose when including the initial 12-week taper period.
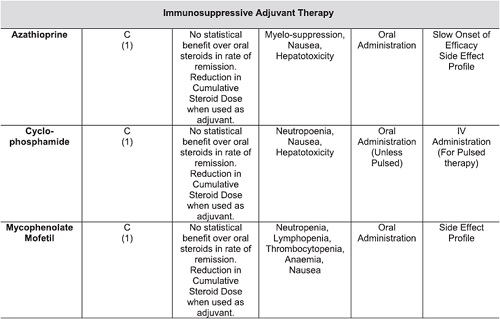
Safety comparison between azathioprine, mycophenolate, and cyclophosphamide
Comparison of the steroid-sparing capacities of azathioprine, mycophenolate, and cyclophosphamide has shown no significant benefit or detriment of one particular treatment over another with the evidence available at hand.
Drug safety is another aspect to take into consideration when choosing an appropriate therapeutic modality. Cyclophosphamide carries significant health risks, including fertility issues and long-term cancer risks.
Azathioprine has risks of hepatotoxicity and myelosuppression, which are also side effects shared with mycophenolate mofetil and cyclophosphamide .
In terms of cost, mycophenolate is more expensive than azathioprine an cyclophosphamide.
This can be a disincentive to the patients who pay for, and the health care providers who may subsidize, these medications.
Expert opinion often recommends the avoidance of cyclophosphamide for safety reasons.
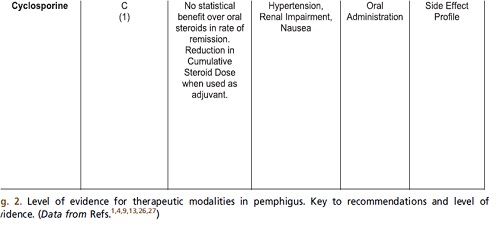
Cyclosporine
Cyclosporine has been evaluated in 2 small RCTs, including comparisons with glucocorticoids alone (including prednisone and methylprednisolone) and cyclophosphamide.
No significant difference was demonstrated for the efficacy of cyclosporine compared with cyclophosphamide or in remission, disease control, or rates of relapse.
There was no difference observed in the cumulative glucocorticoid dose when compared with placebo control .
Moreover, there was no difference observed in any clinical outcome, including remission, disease control, or relapse when cyclosporine was compared with glucocorticoids alone.
Antiinflammatory Therapies Dapsone
Dapsone is a chemotherapeutic agent theorized to function as an antiinflammatory therapy through inhibiting myeloperoxidase resulting in antineutrophilic activity.
Martin and colleagues’ 2009 systematic review identified 1 placebo-controlled RCT in which the effect of dapsone as a thirdline adjuvant agent in pemphigus was examined.
It included 19 PV and PF participants who were twice unable to taper their prednisone lower than 15 mg/d using a predefined tapering schedule.
The steroid-sparing effect of dapsone was inconclusive because the study was underpowered.
The effect of dapsone on the rate of remission and withdrawal caused by adverse events was also inconclusive.
Sulfasalazine and pentoxifylline
El-Darouti and colleagues published a RCT in 2009 concerning the efficacy of sulfasalazine and pentoxifylline as low-cost antiinflammatory drugs to control PV.
All 64 patients in the study were initiated on 500 mg of an oral glucocorticoid and 100 mg of cyclophosphamide. Forty-two patients also received 500 mg sulfasalazine TDS and 400 mg pentoxifylline TDS with the remaining enrolled patient receiving placebo.
The difference between the 2 groups at 8 weeks regarding clinical improvement (as rated by a blinded dermatologist) was statistically significant (P<.001) favoring the intervention group.
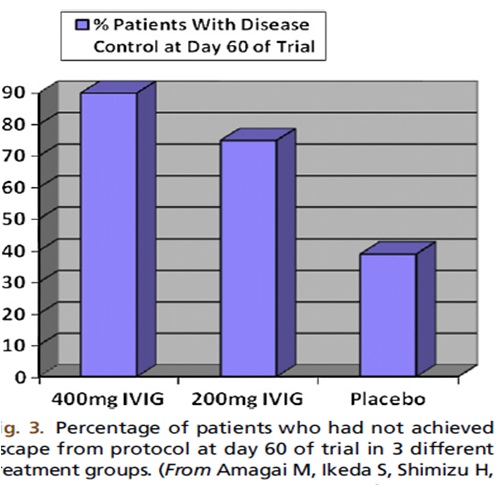
Intravenous immunoglobulin
Intravenous immunoglobulin (IVIG) has been used as one component of combined therapy for severe pemphigus since 1989.
A recent randomized trial by Amagai and colleagues examined the efficacy of a single-cycle of adjuvant IVIG in the management of pemphigus in 61 participants.
The primary outcome measure reported was time to escape from protocol, which is akin to duration of response.
Their results revealed a benefit in duration of response in the 400 mg IVIG treatment group when compared with placebo (P<.001).
The comparison between the 200-mg IVIG treatment group and the placebo group showed weak evidence of effect , although it demonstrates a dose-response relationship for IVIG (Fig. 3).
There was also a benefit in pemphigus activity score and antibody titre demonstrated with IVIG.
Plasmapheresis
Guillaume and colleagues presented the results of a study of 40 participants investigating the efficacy of plasmapheresis in pemphigus. There was no difference in any outcome in this study, including disease control, cumulative steroid dose,or serum antibody titres.
Four individuals of the 22 composing the intervention cohort died of thromboembolism or infection and no deaths were reported in the control group. Although the difference between mortality rates was not calculated to be statistically significant , it is, nevertheless, concerning.
It is unclear if the mortality in this study was related to disease or protocol-related factors. Since that time, no further RCTs evaluating the efficacy of this modality in pemphigus have been reported.
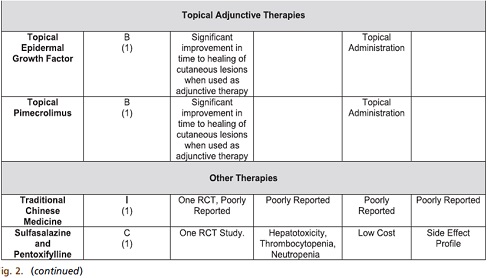
Topical Therapies
Topical epidermal growth factor
Tabrizi and colleagues present one study examining the effect of topical epidermal growth factor on healing time of cutaneous lesions in PV and PF when compared with a control cream (topical silver sulfadiazine [SSD]).
Reanalysis of this data with survival analysis techniques demonstrated a benefit of topical epidermal growth factor in time to lesion healing compared with control.
The long-term safety profile of this intervention is not well studied.
Topical pimecrolimus
A recent randomized, double-blind, left-right placebo-controlled study by Iraji and colleagues assessed the effect of adjuvant topical 1% pimecrolimus cream in 11 patients treated with systemic glucocorticoids and azathioprine. Topical 1% pimecrolimus cream decreased the diameter of cutaneous lesions in patients with PV by a mean of 19% at day 30. Comparison with a placebo cream applied to a symmetric lesion on the same patient revealed a significant difference (P<.0001).
PRACTICAL MANAGEMENT OF PEMPHIGUS:
WHAT WE DO BASED ON THE EVIDENCE
Following a confirmed diagnosis of pemphigus, it is the authors’ practice, based on the evidence presented earlier, to prescribe 1 mg/kg/d of oral prednisone while checking patients’ thiopurine methyl transferase (TPMT) activity and other baseline safety investigations (such as full blood count, hepatic and renal function tests, bone density) before azathioprine.
The prednisone dose is stable until patients reach the consolidation phase.
Azathioprine is commenced based on the TPMT activity levels and is chosen initially based on its low cost unless there are contraindications to its use.
Safety bloods and blood pressure are monitored.
After the consolidation phase, the steroids are gradually reduced by 10 mg every week until they reach 40 mg/d. After this, The azathioprine dose is maintained, unless adverse effects arise, until the steroids are tapered to zero. If there are problems with azathioprine, then mycophenolate mofetil at 2 g/d is substituted as the next drug of choice.
If both of these approaches do not work or the pemphigus relapses, IVIG is commenced at 400 mg/d for 3 consecutive days per month for 3 to 6 months; and once stable, the prednisone is tapered.
Rarely rituximab may be used for recalcitrant disease. Methotrexate may also be used as an adjunctive treatment in the place of azathioprine or mycophenolate.
For PF, dapsone is also considered as a first-line agent.
SUMMARY OF FINDINGS
The optimal therapeutic strategy for pemphigus vulgaris and pemphigus foliaceus is not known.
With multiple treatment modalities and regimens available, treatment choice is complex. In addition to the evidence of the efficacy discussed in this review, the adverse effect profile, cost, and patientn comorbidities are also important considerations.
Of the randomized controlled trials that have been conducted, many are limited by small sample sizes.
Systemic glucocorticoids are central to the effective management of pemphigus, although evidence is not clear as to the optimal dose or regimen.
Adjuvant immunosuppressants or modulatory agents have evidence supporting a steroid sparing role; although, no direct benefits have been observed for remission or disease control.
Topical preparations seem to decrease the time required for healing of erosions.
Overall, further trials will contribute additional information to help clarify the optimal treatments for pemphigus.
Any management strategy for individual patients should include consideration of potential benefits and adverse events unique to the individual patient.
آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
زمان بهترین و ارزشمندترین هدیه ای است كه می توان به كسی ارزانی داشت.هنگامی كه برای كسی وقت می گذاریم، قسمتی از زندگی خود را به او میدهیم كه باز پس گرفته نمی شود . باعث خوشحالی و افتخار من است كه برای عزیزی مثل شما وقت می گذارم و امیدوارم كه با راهنماییهای اساتید این رشته واظهار نظر شما عزیزان این سایت آموزشی پر بارتر گردد.