آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
REVIEW
2011 by the American Academy of Dermatology, Incdoi:10.1016/j.jaad.2011.06.032
Definitions and outcome measures for bullous pemphigoid: Recommendations by an international
panel of experts
Introduction
-There have been only a handful of well-designed randomized controlled trials assessing the effectiveness of therapies for BP.
-meta-analysis is a powerful tool that is used to
pool data across trials, when it is difficult to include enough patients to have sufficient power to compare different treatments.
- it is impossible to compare the therapeutic outcomes from the majority these BP studies using meta-analysis, as they have varying definitions and outcome measures.
PURPOSE
to provide appropriate definitions for the various stages of disease activity, define therapeutic end points in BP, and to propose an objective disease extent measure that can be used in clinical trials.
makes the results of trials more comparable
METHODS
-An international BP definitions committee was organized in 2008, at the point when the international pemphigus definitions committee completed its similar
work on pemphigus. expansion of the first committee and convened 7 times over 2 years to discuss the appropriate definitions.
RECOMMENDATIONS
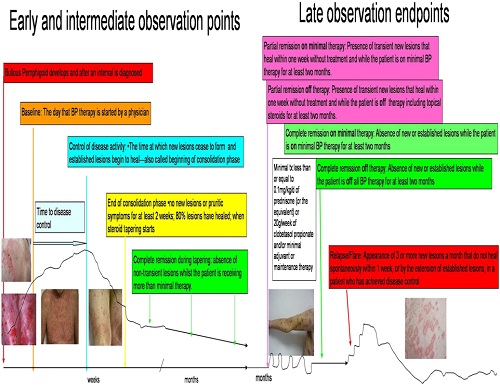
Early end points
Baseline is the point at which a physician starts
treatment for BP.
‘Control of disease activity =disease control;
beginning of consolidation phase. is defined as the
point at which new lesions or pruritic symptoms
cease to form and established lesions begin to heal.
The time to disease control is the time between baseline and this control point.
End of the consolidation phase is defined as the time at which no new lesions or pruritic symptoms have developed for a minimum of 2 weeks and the majority (approximately 80%) of established lesions has healed. Biginning of tapering of corticosteroids
‘‘Transient lesions’’ are new lesions that heal within 1 week or pruritus lasting less than a week and clearing without treatment.
‘‘Nontransient lesions’’ are new lesions that do not heal within 1 week or pruritus continuing more than a week with or without treatment.
Intermediate end points
During this period, the corticosteroids and other treatments are usually being tapered, but for some patients medication doses do not change because of flaring with attempts to taper treatment.
‘‘Complete remission during tapering’’ is the absence of nontransient lesions while the patient is receiving more than minimal therapy. There is no minimum time point here as the patient is under control but has not yet reached the desired outcome of disease remission on minimal or no therapy.
Late observation end points
Late observation end points of disease activity are identified as:
. ‘‘Complete remission off therapy’’ is defined as an absence of new or established lesions or pruritic symptoms while the patient is off all BP therapy for at least 2 month.
‘‘Complete remission on therapy’’ is defined as the absence of new or established lesions or pruritus while the patient is receiving minimal therapy for at least 2 months.
‘‘Partial remission off therapy’’ is defined as the
presence of transient new lesions that heal within1 week without treatment and while the patient is off all BP therapy for at least 2 months.
‘‘Partial remission on minimal therapy’’ is defined
as the presence of transient new lesions that heal
within 1 week while the patient is receiving minimal therapy.
A newer term, ‘‘mild new activity,’’ refers to fewer than 3 lesions a month (blisters, eczematous lesions, or urticarial plaques) that do not heal within 1 week, or the extension of established lesions or pruritus once per week but less than daily, in a patient who has achieved disease control.
This term was not included in the pemphigus definitions but the committee thought that it might be important to capture this phase during studies to determine if some patients with BP and certain characteristics or treatments experienced new mild activity not significant enough to constitute a flare.In this way, it could be determined in the future if these patients with BP might benefit from a change of treatment plan or not.
‘‘Minimal therapy’’is defined as less than or equal to 0.1 mg/kg/d of prednisone (or the equivalent) or 20 g/wk of clobetasol propionate and/or minimal adjuvant or maintenance therapy for at least 2 months.
Minimal adjuvant therapy in BP corresponds to the following doses or less: methotrexate 5 m g/wk; azathioprine 0.7 mg/kg/d mycophenolate mofetil 500 mg/d; mycophenolic acid 360 mg/d; or dapsone 50 mg/d. There has only been one small randomized controlled trial on tetracycline and niacinamide, which was underpowered because of low numbersand was unable to demonstrate a difference .Nevertheless, the committee’s expert opinion is that full therapeutic doses of the tetracyclines may work in localized forms of BP. As the tetracyclineclass of drugs is relatively nontoxic, the full therapeutic dose was listed among minimal therapiesfor BP.
Relapse/flare
The terms ‘‘relapse’’ and ‘‘flare’’ are use interchangeably
and are defined as the appearance of 3 or more new lesions a month (blisters, eczematouslesions, or urticarial plaques) or at least one large ([10 cm diameter) eczematous lesion or urticarial plaque that does not heal within 1 week,or the extension of established lesions or daily pruritus in a patient who has achieved disease control.
Treatment failure
‘‘Failure of therapy for initial control’’ is defined as the development of new nontransient lesions or
continued extension of old lesions, or failure of established lesions to begin to heal or daily pruritus
despite certain strengths of corticosteroids with or without higher doses of adjuvants.
The dose of prednisone defined as treatment failure is 0.75mg/kg/d equivalent for minimum of 3 weeks. This dose was selected because the Cochrane review of interventions for BPdetermined that in acute BP there was no purpose in using prednisone at a higher dose than this. Topical clobetasol propionate at 40g/d for 4 weeks was selected on the basis of the randomized controlled trials conducted by the French group Other therapies include tetracyclineat full doses for 4 weeks; dapsone 1.5 mg/kg/d for 4weeks; methotrexate 15 mg/wk (if [60 kg and no major renal impairment) for 4 weeks; azathioprine2.5 mg/kg/d for 4 weeks (if thiopurine s-methyltransferaselevel is normal); or mycophenolate mofetil 40mg/kg/d (if normal renal function, otherwise according to age/creatinine clearance) for 4 weeks. The definition does not imply these drugs and their respective doses are equivalent in therapeutic efficacy. Rather it provides a standardized agreement as to what can be defined as a failure of therapy.
BP disease activity index
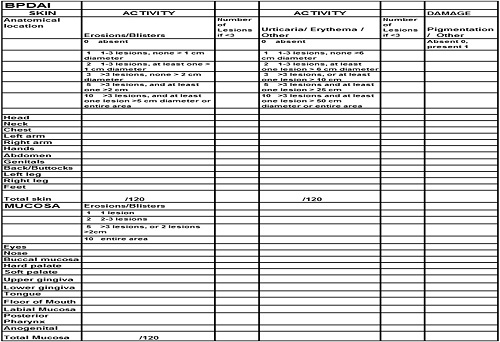
Like the Pemphigus Disease Area Index (PDAI),the BP Disease Area Index (BPDAI) measure has separate scores for skin and mucous membrane activity.
Damage scores are separate as well and are included to remind physicians that not all visible lesions in BP represent active disease. Areas of the skin predominantly affected in BP were taken into account when selecting the skin sites so that trials would better differentiate clinical response in BP. Hence, additional weighting was given to the arms and legs and less emphasis to the face and scalp,slightly different from the PDAI. The mucous membraneareas were retained from the PDAI even though it is relatively rare to see mucous membrane involvement in BP, so that the activity could be compared with extent of mucous membrane involvement in different autoimmune bullous diseases. There are separate columns for the extent of blistering and for the urticarial/eczematous lesions that may be more extensive in BP.
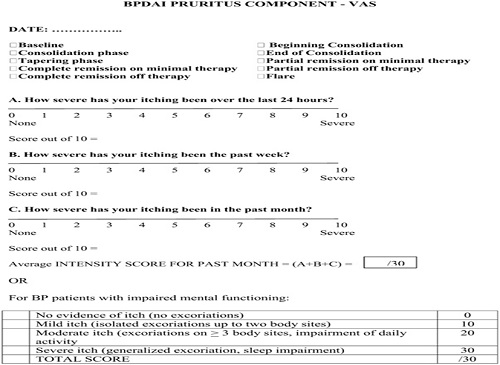
As a major symptom that may herald the onset and recurrence of BP is pruritus, a separate subjective component of the BPDAI is proposed to measure the severity of this . Naturally, other causes of pruritus in the elderly must be excluded, such as xerosis, dermatitis, renal impairment, liver impairment, and scabies.
Providing that only pruritus related to BP is considered in the definitions and scored, this system can be used to subjectively grade the intensity of pruritus using a visual analog scale to answer the question, ‘‘How severe is your itching today?’’ and the patient marks an ‘‘x’’ on the 0- to 10-cm line where 0 is no itch and 10 is maximal itching . The degree of itching is measured as the distance in centimeters from 0, out of 10. This is repeated for these verity overall of itching in the past week and month. A total score is calculated from this out of 30. If the patient with BP is incapable of completing a reliable visual analog scale rating, for example, as a result of dementia, then the degree of pruritus is inferred based on the extent of excoriations alone, also scored out of 30 . This subjective itch score will not be combined with the objective part of the BPDAI . Eventually, a quality-of-life tool for BP will be necessary as well. The BPDAI will be undergoing validation studies, similar to the partial validation done thus far with the PDA.
DISCUSSION AND CONCLUSION
Despite many trials evaluating therapeutic options for BP, it has been difficult to compare the results from these trials because of the large number of end points and definitions of disease. The formation of an international committee of bullous disease experts able to meet face to face on a regular basis has provided a mechanism for developing with agreed-upon common definitions, and the ongoing discussion and refinement of proposed common measurements for patients with BP, are the initial and necessary steps toward progress in the clinical evaluation and therapy of BP. Further progress and advancement will require a continued unified effort.
آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
زمان بهترین و ارزشمندترین هدیه ای است كه می توان به كسی ارزانی داشت.هنگامی كه برای كسی وقت می گذاریم، قسمتی از زندگی خود را به او میدهیم كه باز پس گرفته نمی شود . باعث خوشحالی و افتخار من است كه برای عزیزی مثل شما وقت می گذارم و امیدوارم كه با راهنماییهای اساتید این رشته واظهار نظر شما عزیزان این سایت آموزشی پر بارتر گردد.