آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
ase 1
A 15 year old girl with pruritic lesions since 40 days ago






Differential Diagnosis
DH
Ig A pemphigus
Pemphigus herpetiformis
Linear Ig A bullouse dermatosis
Your diagnostic plan???
Biopsy
DIF
Desmogelin Elisa
Pemphigus herpetiformis
Most patients with herpetiform pemphigus have a clinical variant of pemphigus foliaceus the remainder may have a variant of pemphigus vulgaris.
This disorder is characterized by:
( 1) erythematous urticarial plaques and tense vesicles that present in a herpetiform arrangement;
(2) eosinophilic spongiosis and subcorneal pustules with minimal or no apparent acantholysis histologically;
(3) IgG autoantibodies directed against the cell surfaces of keratinocytes50
The target antigen is Dsg1 in most cases and Dsg3 in the remainder. Some patients with herpetiform pemphigus will have features of pemphigus foliaceus or vulgaris during the course of their disease,
It is assumed that the pathogenic blister-inducing activity of the IgG autoantibodies in herpetiform pemphigus might be weaker than that seen in classic forms of pemphigus.
Although often clinically less severe than pemphigus vulgaris, the course may be more chronic.



Case 2
A 42 year man presenting with alopetic patches with overlying agminated keratotic spinous prifolicular papules discreted over the limbs, scalp and musta Since 2 years ago


DD
Alopecia mucinosa (folicular mucinosis)
LP
Prifolicular MF
Lichen spinolosa
Folicular Mucinosis
This uncommon inflammatory disorder, described in 1957 by Pinkus, has a predilection for children and for adults in the third and fourth decades of life
Although follicular keratinocytes have been considered to be the source of the mucin, an etiologic role for cell-mediated immune mechanisms has been proposed, including a reaction to persistent antigens such as Staphylococcus aureus.
Primary folicular mucinosis
Acute or subacute eruption in children and young adults characterized by one or several pink plaques (that sometimes have associated scale) or plaques composed of grouped follicular papules.
Lesions are limited to the face and scalp and are associated with alopecia.
Papulonodules, annular plaques, folliculitis, follicular spines and acneiform eruptions have also been described.
Secondary folicular mucinosis
( 1) a more generalized distribution (extremities, trunk and facei
(2) larger and more numerous plaques
(3) a chronic clinical course
(4) Occurrence in a slightly older age group, associated with atopic dermatitis or cutaneous T-celllymphoma, rather than a primary condition
Pathology
Mucin accumulates within the follicular epithelium and sebaceous glands, causing keratinocytes to disconnect
In more advanced lesions, the follicles are converted into cystic spaces containing mucin, inflammatory cells and altered keratinocytes.
A perifollicular infiltrate of lymphocytes, histiocytes and eosinophils is seen
The differentiation between primary follicular mucinosis and mycosis fungoides-associated follicular mucinosis is very difficule, and there is no single reliable criterion
features in favor of a primary form are
the young age of the patient,
a solitary plaque or limited number of lesions in the head and neck region,
spontaneous resolution,
the absence histologically of epidermotropism and atypical lymphocytes.
Detection of clonal T-cell gene rearrangements does not seem to help differentiate the two types
Treatment
A wait-and-see approach is recommended for primary follicular mucinosis as many cases resolve spontaneously within 2-24 months.
Based upon case series and case reports, topical, intralesional and systemic corticosteroids, PUVA, dapsone, antimalarials, indomethacin, minocycline, oral isotretinoin, interferona- 2b, orthovoltage irradiation, and UVA1 phototherapy have been reported to be beneficial.
For secondary forms, treatment of the underlying disease is indicated.
Longitudinal evaluation and assessment for cutaneous T-cell lymphoma is recommended for patients with presumed primary follicular mucinosis that is persistent or becomes more extensive.
Case 3
A 52 year old woman with an erythematous papule at the nape (back of the neck) since 1 month ago

DD
Leshmaniasis
Sarcoidosis
Adnexal tumor
Spitz nevus
Granolomatouse reaction
Lymphoma, pseudolymphoma
jessner
Lymphocytic infilteration of jessner
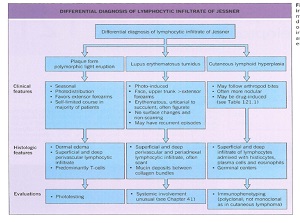
Lymphocytic infiltrate of Jessner occurs primarily in middle-aged adults.
There is no gender predilection.
Some authors believe it is a variant of either lupus erythematosus, cutaneous lymphoid hyperplasia or polymorphic light eruption
while in Europe, it has been associated with Borrelia burgdorferi infection.
There are cases of co-occurrence with LE and with polymorphic light eruption, further raising the possibility that these entities are related.
Lastly, rare cases of drug-induced (e.g. angiotensin-converting enzyme [ACE] inhibitors, glatiramer acetate) have been described
primarily on the head, neck and upper back
as one or several asymptomatic erythematous papules, plaques and, less commonly, nodules, with an absence of secondary changes such as scale
Annular plaques with central clearing are commonly observed
individual lesions last several weeks to months.
There are no associated systemic manifestations.
Emotional stress has been associated with exacerbation of the eruption in a minority of patients.
The eruption resolves spontaneously and without sequelae in most patients.
pathology
There is a superficial and deep, primarily perivascular, lymphocytic infiltrate that may surround hair follicles.
By immunohistochemistry, a mixed T-cell infiltrate with a predominance of CD8+ lymphocytes is seen, admixed with small clusters of CD 123+ plasmacytoid dendritic cells.
An increase in reticular dermal mucin may be seen.
treatment
Oral antibiotics and topical or intralesional corticosteroids have been used with limited success.
Up to 50% of patients may improve with hydroxychloroquine.
In general LIJ is resistant to radiation therapy.
A crossover study of oral thalidomide ( 100 mg/day) versus placebo in 25 patients resulted in a clinical response of 76% for thalidomide and 16% for placebo.
In isolated case reports, improvement following pulsed dye (595 nm) laser treatment or chemotherapy (for an unrelated malignancy) has been described







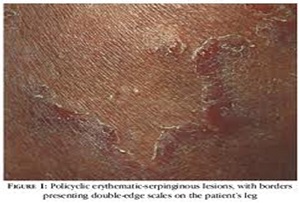
Case 4
A 62 year old woman with one erythematous and firm bilobed papul at the inner cantus of the eye since childhood with recent enlargement

DD
Adnexal tumor
BCC
Apocrine hydrocystoma
Hemangioma
ALHE
Arteriovenus Malformation
Schobinger's staging was adopted by the ISSVA in order to classify AVMs according to their clinical severity.
The stages are:
( 1) quiescent/dormant - macular or slightly infiltrated, red, warm lesions mimicking a PWS ;
(2) expansion - warm masses with throbbing and thrills over dilated draining veins
(3) destruction- necrosis, hemorrhage, ulceration and (occasionally) lytic bone lesions (plus findings of stage 2)
(4) cardiac decompensation (plus findings of stage 2 ± 3).
Initial evaluation with ultrasonography and MRI studies can confirm the diagnosis and delinate the extent of the lesion
In 40% of patients, AVMs are visible at birth; the remainder appear later in life.
The most frequent location is cephalic (-70% of patients in the author's experience;
Puberty (75% of patients), pregnancy (25% of women) and trauma may result in worsening of AVMs
ALHE
Typical lesions involving the dermis and subcutaneous tissue are well circumscribed and show vaguely lobular proliferations of capillary-sized vessels surrounding larger central blood vessels, with a variably dense perivascular inflammatory infiltrate rich in lymphocytes and eosinophils
Cases have been described in association with arteriovenous fistulas and malformations. These findings suggest that in some patients AHE may be reactive, rather than neoplastic, especially in those with this latter type of lesion.
About one-third of lesions recur after excision , sometimes due to incomplete excision of an underlying nidus of arteriovenous (AV) shunting (e.g. an AV malformation, an acquired AV fistula)
Case 5
A 45 year old woman with excorated severely pruritic papules on limbs and trunk since 4 years ago + grouped bulla and vesicles in the axillary since 1 week before.






Pathology
More compatible with lichenoid dermatitis
Epidermal atrophy + vacuolar degeneration of basal layer + band like lymphocytic infiltration + civatte body + melanophages in papilary dermis.
Without hypergranulosis
Case 7
A 17 year old boy
Posterior aspect of the ear
Firm nodul

DD
Keloid
Adnexal tumor
Ortokeratotic keratosis + thick collagen bundles in the derm +discrete inflamatory infilteration + dilated vessels of superficial dermis
Case 8

DD
BCC superficial
Padget‘s disease
Bowen




Case 9
A 18 year old boy
Hyperkeratotic plaques with sharp borders
Some of them crusted
Since 6-7 months ago
Similar lesions at infancy




Pathology
Spongiotic dermatitis
Acantosis, severe spongiosis,
Hyperkeratosis, parakeratosis
Mononuclear infiltration + eosinophil




آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
زمان بهترین و ارزشمندترین هدیه ای است كه می توان به كسی ارزانی داشت.هنگامی كه برای كسی وقت می گذاریم، قسمتی از زندگی خود را به او میدهیم كه باز پس گرفته نمی شود . باعث خوشحالی و افتخار من است كه برای عزیزی مثل شما وقت می گذارم و امیدوارم كه با راهنماییهای اساتید این رشته واظهار نظر شما عزیزان این سایت آموزشی پر بارتر گردد.