آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
Case report
A 9-year-old girl presented to our pediatric dermatology clinic with a cervical plaque that had been present for six months.
She complained of slight pruritus. The plaque had been treated by her primary care physician as neurodermitis with mometasone without improving.
On physical examination a 2.5 cm plaque with mild hyperpigmentation on the posterior aspect of her neck with rounded morphology and elevated borders is noted .

What is your clinical diagnosis?

These clinical features suggested the clinical diagnosis of granuloma annulare . We performed a 4 mm punch biopsy of the lesion to confirm the clinical diagnosis.
Now what is your diagnosis?
Dermatofibroma
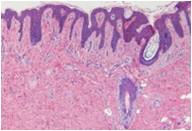
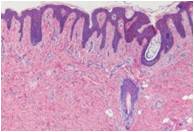
Histologic examination of the specimen showed an ill-defined, uniform spindle cell neoplasm filling the reticular dermis and the superficial part of the hypodermis.
Spindle-cell proliferation seen on a matrix of collagen fibers. The spindled cells are arranged in parallel to the surface of the skin. These cells were distributed forming fascicles or bands.
Bopsy showed a fibrohistiocytic proliferation, which has many diffrerential diagnoses.
The mother of the patient reported the lesion had grown since the last visit. The lesion was excised completely.
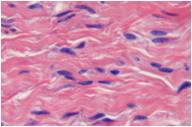
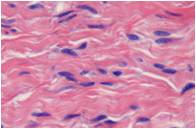
The cells had elongated shape, eosinophilic cytoplasm, and fine nuclear chromatin. Some cells had small nucleoli. The cells lacked mitoses. Adnexal structures were spared. Orcein staining showed abundant elastic fibers.
Immunohistochemical evaluation showed that the spindle-shaped cells reacted positively for vimentine and there was no reactivity with actin, desmin, factor XIIIa, S-100, CD34, and CD68
Based on these histologic and inmunohistologic features, the diagnosis was compatible with dermatomyofibroma, which was completely excised. The patient has shown no signs of recurrence after 1 year of follow-up.
Discussion
Dermatomyiofibroma represents a relatively rare cutaneous mesenchymal neoplasm of fibroblastic/myofibroblastic differentiation.
The fibrohistiocytic tumors of the skin are a heterogeneous group of dermal/subcutaneous mesenchymal neoplasms which show fibroblastic, myofibroblastic, and histiocytic differentiation. Dermatomyofibroma was first described by Hügel in 1991 under the name, plaque-like dermal fibromatosis .One year later it was described by Kamino under the name dermatomyofibroma. The latter name has also become accepted in Europe].
Dermatomyofibroma is a solitary, slowly growing and benign tumor. Cases have been reported with multiple dermatomyofibromas in a single anatomical area. It is primarily found in young adult females and in preteen children. The dermatomyofibroma is more common in women than in men. The average age of presentation in women is 31.4 years and men 12.3 years. There are case reports of male patients as young as one year old..
It is remarkable that the affected females are significantly older than the affected males. The cause of this difference in sex and age distribution is not clear. Possibly dermatomyofibroma may regress spontaneously after childhood in males. The tendency of dermatomyofibroma to occur in postpubescent females and prepubescent males may indicate that this tumor could be responsive to hormones, as has been suggested by some authors .More studies are needed to elucidate the characteristic distribution of gender and age.
Dermatomyofibroma presents clinically as a plaque or nodule, more palpable than visible. In the literature there are annular or linear variants that are rare . The overlying surface can be slightly pigmented. Normally the dermatomyofibroma is small, usually measuring 1 to 2 cm in diameter, although there have been reported cases of giant dermatomyofibromas. The sites of predilection are the anterior abdominal wall in adult women, the posterior neck in prepubertal boys, and the shoulder and axilla in both genders.
The clinical differential diagnosis includes dermatofibroma, granuloma annulare, pseudolymphoma cutis, hypertrophic scar, cyst, and connective tissue nevus.
Histological examination shows an ill-defined, uniform, spindle-cell proliferation on a matrix of collagen fibers in the dermis with a parallel arrangement to the skin surface. These spindle cells show fibroblastic and myofibroblastic differentiation. The cytoplasm is pale, eosinophilic, and ill-defined. The nuclei are elongated and well-defined. On the other hand, mitotic figures are rarely seen. Spindle cells are arranged to form well-defined fascicles. Collagen fibers are thin, crisscross between the spindle cells, and stain with Masson trichrome. Elastic fibers are not reduced in number, but may be increased in number and even fragmented. This would be a distinctive feature that would help us in the differential diagnosis. Elastic fibers are altered in dermatofibroma, hypertrophic scar, dermatofibrosarcoma protuberans and piloleiomyoma. Elastic fibers stain with orcein and Verhoeff van Gieson .
The clinical differential diagnosis includes dermatofibroma, granuloma annulare, pseudolymphoma cutis, hypertrophic scar, cyst, and connective tissue nevus .
Histological examination shows an ill-defined, uniform, spindle-cell proliferation on a matrix of collagen fibers in the dermis with a parallel arrangement to the skin surface. These spindle cells show fibroblastic and myofibroblastic differentiation. The cytoplasm is pale, eosinophilic, and ill-defined. The nuclei are elongated and well-defined. On the other hand, mitotic figures are rarely seen. Spindle cells are arranged to form well-defined fascicles. Collagen fibers are thin, crisscross between the spindle cells, and stain with Masson trichrome. Elastic fibers are not reduced in number, but may be increased in number and even fragmented. This would be a distinctive feature that would help us in the differential diagnosis. Elastic fibers are altered in dermatofibroma, hypertrophic scar, dermatofibrosarcoma protuberans and piloleiomyoma. Elastic fibers stain with orcein and Verhoeff van Gieson .
Dermatofibroma shows a nodular proliferation of myofibroblasts, fibroblasts, and histiocytic cells presenting a stellate morphology. The dermatofibroma exhibits abundant vascularization and breaches the adnexal structures. Elastic fibers are decreased in number or absent and stain positively for factor XIIIa. When the dermatofibroma has many myofibroblasts is difficult to distinguish from dermatomyofibroma .
Piloleiomyoma is a tumor with more cellularity than dermatomyofibroma and affects the deep dermis. The cells have cigar-shaped nuclei. The center of the lesion has interdigitated fascicles and in the periphery there is an infiltrative pattern. The immunohistochemical features include positivity for desmin and smooth muscle actin .
Neurofibroma is a tumor that is usually solitary, affecting the superficial dermis. Its component cells are usually spindle cells arranged chaotically on a stroma that is vascular, fibrotic, edematous, or myxedematous. Immunohistochemistry of the tumor is positive for S-100, but CD34 can be positive or negative.
The connective tissue nevus presents a very subtle clinical appearance that can be confused with normal skin. Histopathologically is an ill-defined area of increased dermal collagen that shows a normal number of fibroblasts. Elastic fibers may be increased, decreased, or normal in number. Dermal fibromatosis is difficult to distinguish from a small biopsy of dermatomyofibroma.
Dermal fibromatosis presents as poorly demarcated dermal and subcutaneous nodules or plaques, which are formed by bundles of fibroblasts and myofibroblasts. In dermal fibromatosis there may be a hypocellular focus with thick collagen fibers and there may be a hypercellular focus with thin collagen fibers. The skin can invade the aponeurosis, adjacent fascia, and skeletal muscle
Fibrous hamartoma of infancy and plexiform fibrohisticytic tumor are two rare soft tissue neoplasms of childhood and young adulthood, which are in the differential diagnosis. Both lesions are located in the subcutaneous tissue and rarely affect the dermis. On the contrary, dermatomyofibroma is generally affecting the dermis and sometimes can affect the superficial subcutaneous tissue.
Dermatomyofibromas have not been reported to recur or metastasize. The treatment of choice for dermatomyofibroma is total excision of the lesion and it has a good prognosis.
It is important to establish the diagnosis of this entity. The dermatomyofibroma must be distinguished from other fibrohistiocytic tumors of intermediate or malignant nature.
آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
زمان بهترین و ارزشمندترین هدیه ای است كه می توان به كسی ارزانی داشت.هنگامی كه برای كسی وقت می گذاریم، قسمتی از زندگی خود را به او میدهیم كه باز پس گرفته نمی شود . باعث خوشحالی و افتخار من است كه برای عزیزی مثل شما وقت می گذارم و امیدوارم كه با راهنماییهای اساتید این رشته واظهار نظر شما عزیزان این سایت آموزشی پر بارتر گردد.