آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
CASE 1
A 27-year-old married lady, resident of Tamil Nadu (South India), was admitted to the ICU with complaints of low grade fever, weakness, dyspnea on accustomed exertion, swelling of face, hands and feet of 15 days duration.
She developed blisters on the skin and mucosal ulcers four days later and was referred to a dermatologist. Skin examination revealed diffuse periorbital edema, multiple tense vesiculobullous lesions on the face, eyelids, neck, trunk and external genitalia ,Both Nikolskiy and bulla spread signs were negative. Besides, there were multiple painful ulcers on the lips and buccal mucosa

CASE 2
A 65-year-old man developed skin fragility and blistering across the dorsum of the hands while on holiday in Spain, a country he visited regularly
his medications of tiotropium, irbesartan, simvastatin with ezetimibe, cetirizine, aspirin and oxprenolol for many years. Three days before travel, he had been started on a 2-week course of ciprofloxacin for a chest infection
He reported a heavy alcohol intake

CASE 3
A 55-year-old black female on hemodialysis (HD) for 3 years complained of progressive facial hyperpigmentation associated with facial hirsutism of 6 months duration. The primary etiology of her renal failure was hypertension. She was hepatitis C positive and denied alcohol abuse. She subsequently developed painful blisters on her hand that burst spontaneously

porphyria cutanea tarda
Classified Into :
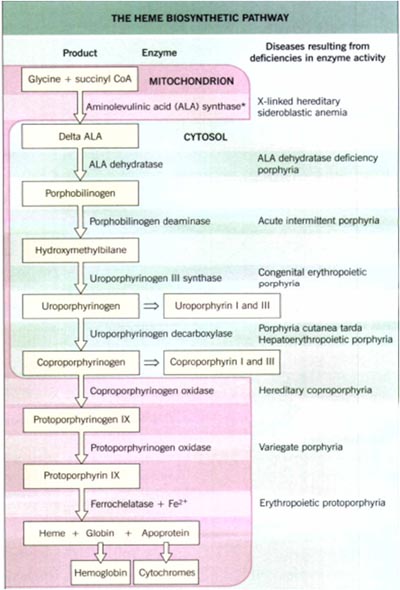
erythropoietic and hepatic :according to the major site of expression of the enzyme deficiency
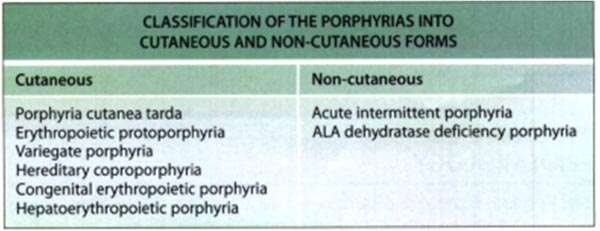
cutaneous versus non-cutaneous forms
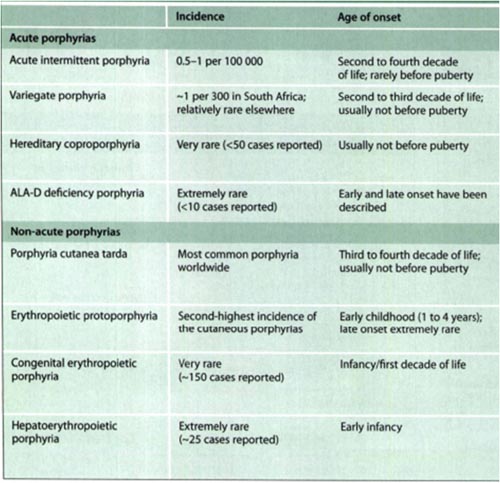
acute and non-acute: presence or absence of potentially life-threatening acute neurologicattacks
Porphyrins absorb light intensely in the Soret band (major absorption peak between 400 and 410 nm).
By absorbing this radiant energy, these molecules then enter into an excited state. Excited porphyrins in their singlet and triplet states can transfer this absorbed energy to oxygen molecules, thereby creating reactive oxygen species.
Cellular and tissue damage induced by photoactivated porphyrins is believed to result primarily from the formation of reactive singlet oxygen and free radicals, with subsequent lipid peroxidation and protein cross-linking
The type of cellular damage depends on the solubility and tissue distribution of the porphyrins.
Accumulation of water-soluble uro-, copro- and protoporphyrins leads to blistering, as is seen in most of the cutaneous porphyrias (e.g. porphyria cutanea tarda, variegate porphyria, hereditary coproporphyria).
In contrast, accumulation of lipophilic protoporphyrins leads to an immediate cutaneous burning sensation after exposure to UV light, accompanied by erythema and edema, as is seen in erythropoietic protoporphyria.
Porphyria Cutanea Tarda
the most common type of porphyria.
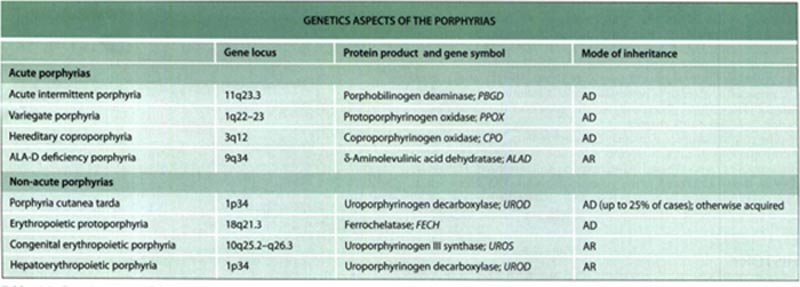
decreased catalytic activity of uroporphyrinogen decarboxylase, the fifth enzyme
Depending upon the major site of expression of the uroporphyrinogen decarboxylase, at least two types of PCT can be distinguished:
type I ,sporadic (acquired) variant, in which the enzymatic deficiency is exclusively expresse in the liver
type II ,An autosomal dominant familial (hereditary) variant, in which the catalytic enzymatic defect is detected in all tissues
Currently, the ratio of type I to type II PCT is estimated to be approximately 3: 1 to 4: 1
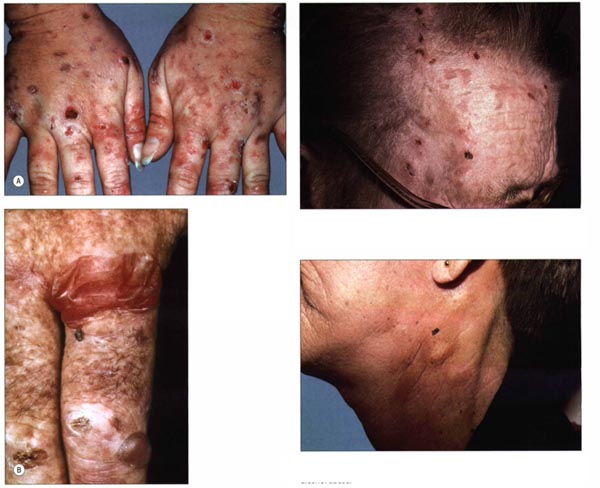
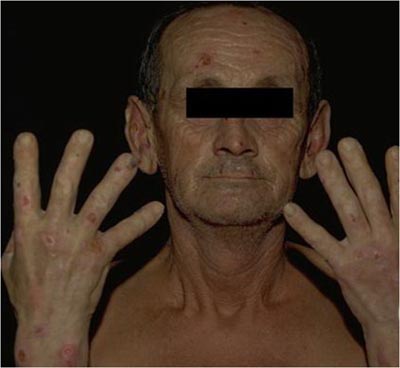
cutaneous manifestations :




Triggering Factors:
alcohol, estrogens, polychlorinated hydrocarbons, hemodialysis in patients with renal failure, iron, inheritance of specific mutations (C282Y and H63D) in the HFE gene which underlie classic hemochromatosis, and viral infections such as hepatitis C and HIV
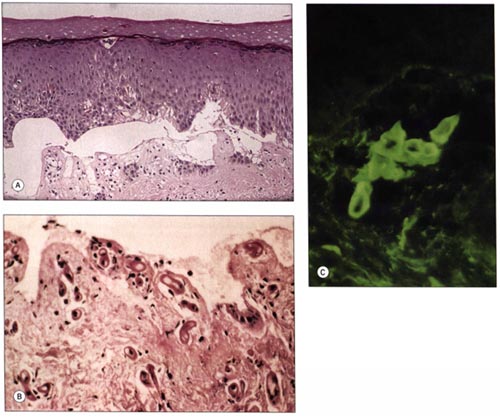
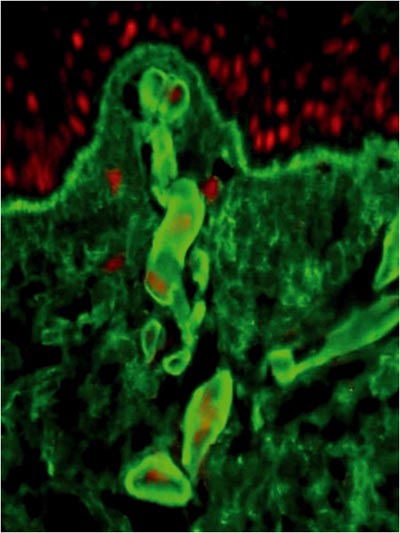
Histologic examination of vesiculobullae commonly reveals:
subepidermal cell-poor blisters
characteristic festooning of dermal papillaej
deposition of PAS-positive glycoproteins in and around the wall of vessels localized in the upper dermis
Direct immunofluorescence microscopy
immunoglobulins (mainly IgG, less commonly IgM), complement and fibrinogen at the dermal-epidermal junction and around blood vessels of the papillary dermis
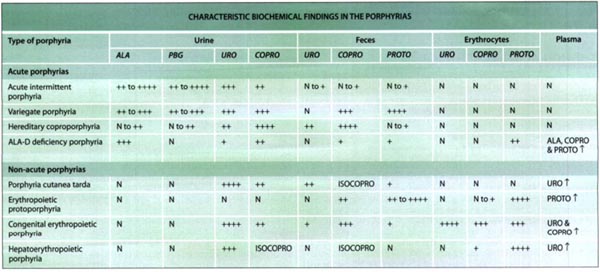
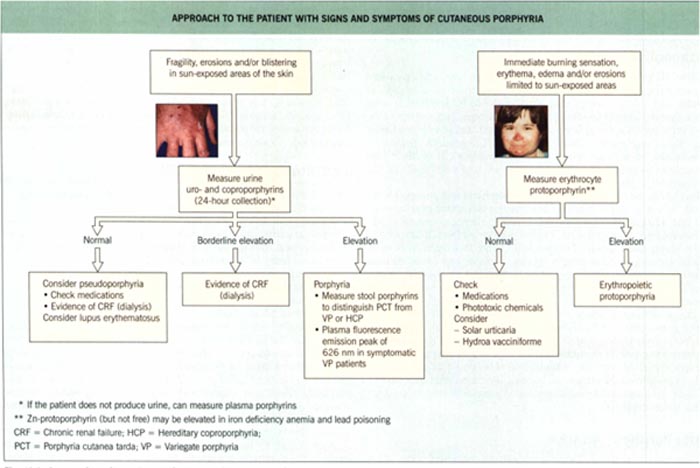
The laboratory investigation that assists in establishing the diagnosis of a specific type of porphyria involves up to four steps:
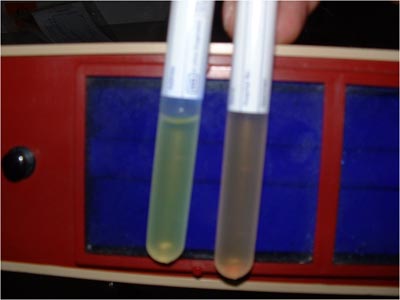
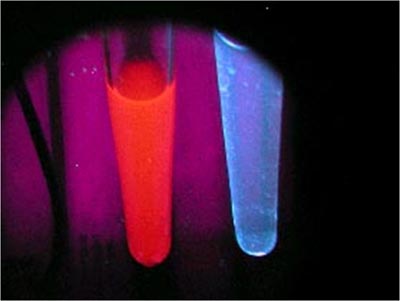
Historically, a presumptive clinical diagnosis of PCT was followed by an examination of the patient's urine, both under Wood's lamp illumination (in the dark) and after exposure to natural light.
the urine of PCT patients turns red to brown after several hours of exposure to natural light and it has a pink to red fluorescence when exposed to a UVA light source.
However, it has to be borne in mind that these bedside observations are neither sensitive nor specific diagnostic tests.
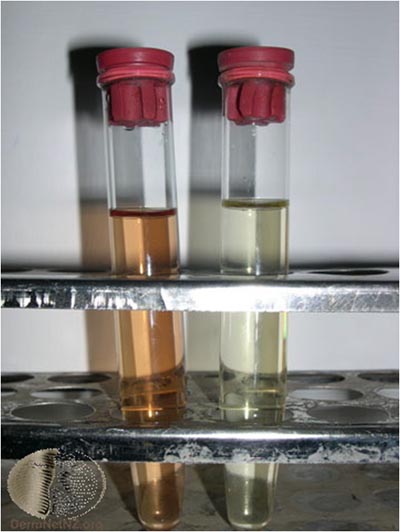
Biochemically,
increased urinary excretion of uroporphyrin, hepta-carboxylated porphyrins ,and coproporphyrin can be detected,
increased excretion of isocoproporphyrin in the feces;
the latter finding being exclusive to PCT (and hepatoerythropoietic porphyria).
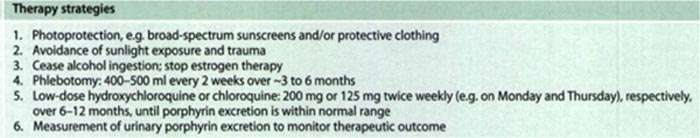
Treatment
Avoidance of UV
sun-protective clothing,
broad-spectrum sunscreens
Because the wavelengths that induce the porphyrias are in the 400-410 nm range, sunscreens are limited in their therapeutic effectiveness, with the exception of titanium dioxide and zinc oxide
eliminate triggering factors such as alcohol ingestion and estrogen therapy
Phlebotomy
In patients with iron overload, successful treatment can be achieved by repeated phlebotomy (venesection) of approximately 500 ml blood every 2 weeks, as tolerated by the patient; some authors recommend weekly venesection of 300 ml blood.
While the therapeutic goal is to reduce serum ferritin levels to the lower limit of the reference range, care should be taken to not induce anemia.
Phlebotomy usually leads to resolution of skin fragility and blistering within 2-4 months.
However, normalization of urinary porphyrin concentrations will usually take longer (about 12 months).
When required, maintenance phlebotomy is performed at less frequent intervals.
Antimalarials
Work as:
accelerating the secretion of porphyrins,
may also inhibit porphyrin synthesis.
Standard therapy consists of 200 mg of hydroxychloroquine or 125 mg of chloroquine twice weekly, and complete remission can be expected within 6-9 months
If the initial dose is tolerated but does not control the cutaneous symptoms, the same dosage can be give more frequently, i.e. three to four times weekly.
These antimalarials can be used in combination with phlebotomy to induce a remission more rapidly
CASE 1
A 27-year-old married lady, resident of Tamil Nadu (South India), was admitted to the ICU with complaints of low grade fever, weakness, dyspnea on accustomed exertion, swelling of face, hands and feet of 15 days duration.
She developed blisters on the skin and mucosal ulcers four days later and was referred to a dermatologist. Skin examination revealed diffuse periorbital edema, multiple tense vesiculobullous lesions on the face, eyelids, neck, trunk and external genitalia ,Both Nikolskiy and bulla spread signs were negative. Besides, there were multiple painful ulcers on the lips and buccal mucosa

As the 24h urinary protein was markedly elevated (3.5 g/24 h)
Liver and renal function tests, VDRL, ELISA for HIV, USG abdomen and Mantoux test were within normal limits.
IgG and IgM for Mycobacterium tuberculosis were negative.
Blood samples were sent for ANA and dsDNA
Histopathology of the skin showed necrotic keratinocytes and subepidermal vesicle, which were teeming with neutrophils and a few eosinophils.
DIF study revealed IgG deposits at the DEJ
Diagnosis:
Bullous SLE
Both ANA and dsDNA were strongly positive. The patient was diagnosed as a case of bullous SLE based on the following ACR criteria; oral ulceration, pleural and pericardial effusion (serositis), proteinuria >3.5 g/day, positive ANA and positive dsDNA.
CASE 2
A 65-year-old man developed skin fragility and blistering across the dorsum of the hands while on holiday in Spain, a country he visited regularly
his medications of tiotropium, irbesartan, simvastatin with ezetimibe, cetirizine, aspirin and oxprenolol for many years. Three days before travel, he had been started on a 2-week course of ciprofloxacin for a chest infection
He reported a heavy alcohol intake

On examination, the patient had one intact blister and several ulcerated lesions across the dorsum of the hands No scarring or milia were seen. A provisional diagnosis of porphyria cutanea tarda was made,
Investigations revealed a normal full blood count and renal profile. There were raised levels of alanine transaminase (48 IU ⁄ L; normal range 0–41) and c-glutamyl transferase (77 IU ⁄ L; normal range 8–61). The ferritin level was normal and hepatitis C serology was negative. Plasma porphyrins were not detected, and urinary, faecal and red-cell porphyrins were not in excess when measured by fluorescence emission spectroscopy.
A punch biopsy was taken, which revealed an ulcer edge consistent with a healing wound. Direct immunofluorescence found bright blood-vessel and hyaline-mantle staining with IgG and a lesser degree of staining with IgA, C3 and fibrinogen
Diagnosis is:
Pseudoporphyria
Pseudoporphyria is an uncommon rash that can develop following increased exposure to ultraviolet (UV)A in patients taking various drugs or on haemodialysis.
Our patients rash developed on holiday; however, he had not had any reaction on the other trips abroad.
Although the increased UVA exposure may have contributed to the development of pseudoporphyria, we believe it cannot be the only trigger in this case.
The patient had been stable on his medication for many years and it was felt unlikely that these were to blame.
The only new medication was ciprofloxacin.
CASE 3
A 55-year-old black female on hemodialysis (HD) for 3 years complained of progressive facial hyperpigmentation associated with facial hirsutism of 6 months duration. The primary etiology of her renal failure was hypertension. She was hepatitis C positive and denied alcohol abuse. She subsequently developed painful blisters on her hand that burst spontaneously

Liver enzymes were elevated (AST 95U/L, ALT 63U/L, AP 891U/L).
Microscopic examination revealed hyperkeratosis (consistent with the anatomic site) and subepidermal blistering with festooning of dermal papillae. A mild, mixed inflammatory infiltrate including neutrophils was present
Diagnosis:
Porphyria Cutanea Tarda
Her predialysis serum porphyrin level was >2000 nmol/L.
Serum ferritin was 2625 ng/mL
Based on clinical, biochemical, and histopathological findings, a diagnosis of sporadic PCT was made
Treatment with oral hydroxychloroquine was instituted and her HD membrane was changed from low flux to high flux.
Instead of regular phlebotomy to decrease iron overload,
Erythropoietin therapy was adjusted to maintain the hemoglobin between 10 and 12 g/dL.
Iron supplementation was discontinued.
After 2 months of therapy, improvement of her blisters was noted.
Facial hirsutism and hyperpigmentation also improved, but to a lesser degree.
A few months later, the blisters resolved (Figure 2) and the serum porphyrin level decreased to 1400 nmol/L

آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
زمان بهترین و ارزشمندترین هدیه ای است كه می توان به كسی ارزانی داشت.هنگامی كه برای كسی وقت می گذاریم، قسمتی از زندگی خود را به او میدهیم كه باز پس گرفته نمی شود . باعث خوشحالی و افتخار من است كه برای عزیزی مثل شما وقت می گذارم و امیدوارم كه با راهنماییهای اساتید این رشته واظهار نظر شما عزیزان این سایت آموزشی پر بارتر گردد.