آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
Life Threatening Dermatoses
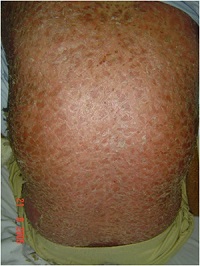
Erythroderma
Toxic Epidermal Necrolysis
Stevens Johnson Syndrome
Autoimmune Bullous Disease
Urticaria & Angioedema
اریترودرمی

Nursing considerations
▪ Monitor and replace fluids and electrolytes, especially in patients with burns or widespread erythema.
▪ Withhold all medications until the cause of the erythema has been identified.
▪ Administer an antibiotic and a topical or systemic corticosteroid as ordered.
▪ For the patient with itching skin, give soothing baths or apply open wet dressings containing starch, bran, or sodium bicarbonate.
▪ Administer an antihistamine and analgesic as needed.
▪ For a burn patient with erythema, immerse the affected area in cold water, or apply a sheet soaked in cold water to reduce pain, edema, and erythema.
▪ Prepare the patient for diagnostic tests, such as skin biopsy to detect cancerous lesions, cultures to identify infectious organisms, and sensitivity studies to confirm allergies.
▪ Have the patient with leg erythema keep his legs elevated above heart level.
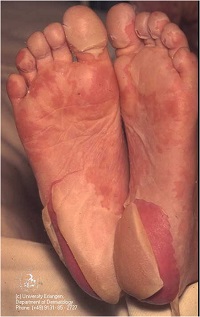
نکرولیز اپیدرمال سمی


Toxic Epidermal Necrolysis (TEN) is a severe skin disorder characterised by separation of the dermal-epidermal junction, as it is observed in second degree superficial burns, and it may also involve any mucosal surface area (otic, buccal, conjunctival, respiratory, genital). This condition is generally induced by the ingestion of drugs, particularly certain antibiotics, nonsteroidal antiinflammatory drugs, and antiepileptic drugs. Mortality has decreased over the last decades, from 80% to about 25% in recent series.
This improvement in survival rate has been related to early diagnosis, management in specialized burn units, proper immunosuppressive treatment and intensive specialised nursing care.
The main nursing diagnosis include abnormalities in the skin and mucose membranes integrity,
risk of infection
loss of blood volume
risk of hypothermia
acute pain
upper airway insufficiency and anxiety.
We emphasize the daily skin and mucose membranes care, and the prevention of conjunctival sinequiae, including daily conjunctival cleaning and debridement of necrotic tissue and fibrin debris using a handle needle



سندروم استیونس جانسون




پمفیگوس ولگاریس



کهیر


Action stat!
In an acute case of urticaria, quickly evaluate respiratory status, and take the patient's vital signs. Ensure patent I.V. access if you note any respiratory difficulty or signs of impending anaphylactic shock. Also, as appropriate, give local epinephrine or apply ice to the affected site to decrease absorption through vasoconstriction. Clear and maintain the airway, give oxygen as needed, and institute cardiac monitoring. Have resuscitation equipment at hand, and be prepared to begin cardiopulmonary resuscitation. Endotracheal intubation or a tracheostomy may be required.
Anaphylaxis.Anaphylaxis—an acute allergic reaction—is marked by the rapid eruption of diffuse urticaria and angioedema, with wheals ranging from pinpoint to palm-size or larger. Lesions are usually pruritic and stinging; paresthesia commonly precedes their eruption. Other acute findings include profound anxiety, weakness, diaphoresis, sneezing, shortness of breath, profuse rhinorrhea, nasal congestion, dysphagia, and warm, moist skin


Nursing considerations
▪ Apply a bland skin emollient or one containing menthol and phenol to the patient's skin.
▪ Administer an antihistamine, a systemic corticosteroid or, if stress is a suspected contributing factor, a tranquilizer, as ordered.
▪ Provide tepid baths and cool compresses to enhance vasoconstriction and decrease pruritus.
▪ Administer oxygen and monitor respiratory status.
آنژیوادم



Patient teaching
▪ Explain the underlying disorder and treatment plan.
▪ Teach the patient to avoid the causative stimulus, if identified.
▪ Emphasize the importance of wearing medical identification for allergies.
▪ Explain signs and symptoms that require prompt medical attention.
▪ Stress ways to avoid anaphylaxi
آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
زمان بهترین و ارزشمندترین هدیه ای است كه می توان به كسی ارزانی داشت.هنگامی كه برای كسی وقت می گذاریم، قسمتی از زندگی خود را به او میدهیم كه باز پس گرفته نمی شود . باعث خوشحالی و افتخار من است كه برای عزیزی مثل شما وقت می گذارم و امیدوارم كه با راهنماییهای اساتید این رشته واظهار نظر شما عزیزان این سایت آموزشی پر بارتر گردد.