آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
• DH is a cutaneous manifestation of Gluten sensitivity.
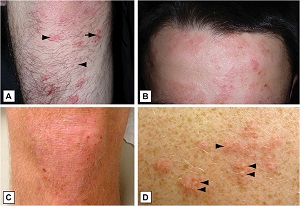
• chronic, polymorphic, pruritic skin disease.
• Typically, young adults present with excoriations only, as the severe pruritus effectively destroys any primary lesions.

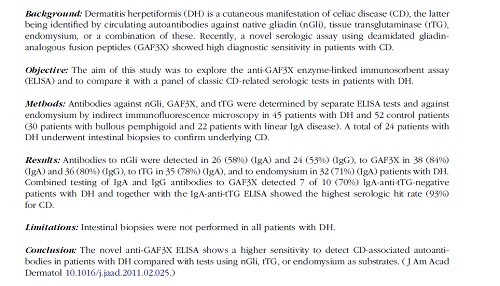
• Tissue transglutaminase (tTG) is the major autoantigen targeted in CD, and epidermal transglutaminase (eTG) is the autoantigen most closely linked to DH.
• IgA anti-eTG is the most sensitive serologic marker for DH.
• Most prevalent in patients of Northern European descent (incidence range of 0.4 to 2.6 per 100,000 people per year )
• DH with onset in childhood tends to be more common in Mediterranean countries.• Rare in Asians ,rarer in African-Americans.
• M> F
• Interestingly, the opposite is true of the prevalence of CD, with female to male ratios ranging from 2:1 to 4:1
• Most patients report the onset of symptoms during the warmer months of the year, any time from spring to late summer
• the most common age range at presentation being 30 to 40 years old. (infancy to the geriatric)
• A complex interplay between autoimmune factors, such as HLA predisposition, genetics, and environment.
Pathogenesis• Twin studies :a concordance rate of 0.91• A population-based analysis of first-degree relatives revealed that the incidence of CD and DH among first-degree relatives was almost 15 times higher than that in the general population.
Pathogenesis• Myosin IXB (MYO9B) on chromosome 9p13
• MYO9B functions in cell signaling and regulation of the actin cytoskeleton dynamics, thereby regulating cell integrity and the permeability of the gut barrier.
• Genomic variants at the interleukin-2 (IL-2) to IL-21 region, regulator of G-protein signaling 1 (RGS1), IL-12A, IL-18 receptor protein (IL18RAP), cluster of chemokine receptor 3 (CCR3), T cell activation GTPaseactivating protein (TAGAP), and SH2B3 protein
• A close association between DH and HLA-DQ2 or HLA-DQ8
• The immunologic basis for development of DH is intimately linked with the pathogenesis of gluten intolerance and CD
• Overt DH is found in only 5–10% of CD patients, conversely CD in only rare incidences of DH
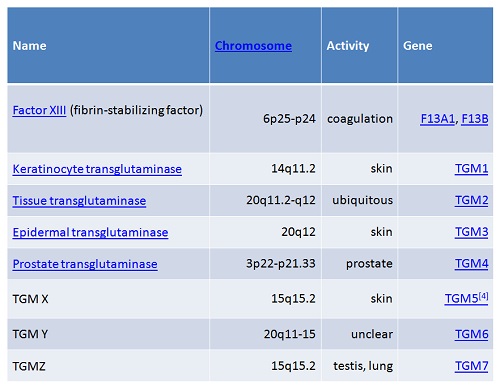
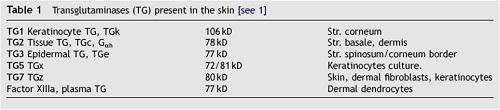
Transglutaminases present in the skin
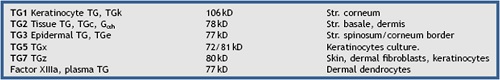
Pathogenesis• tTG :a primarily cytoplasmic, calcium-dependent enzyme that catalyzes cross-links between glutamine and lysine protein residues• Biologic functions : stabilization of the cytoskeleton and extracellular matrix via protein polymerization, the regulation of cell matrix adhesion and cell migration, and proliferation via the effects on integrin-dependent cell signaling
• The expression of eTG is more restricted than tTG, and is primarily seen in the epidermis, small intestine, brain, and testes.
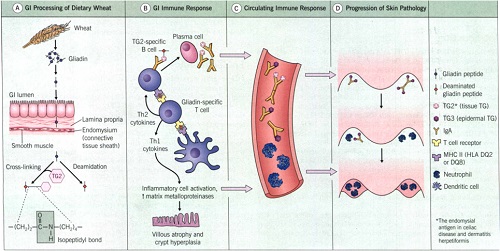
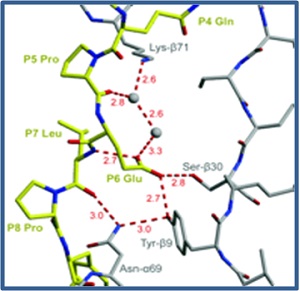
• tTG modifies the alcohol-soluble fraction of gluten known as gliadin into an efficient autoantigen with stronger affinity for HLA-DQ2 on antigen-presenting cells, resulting in T cell stimulation and the ensuing inflammatory responsePathogenesis• Protein-protein crosslinking results in tTG-gliadin complexes that also generate a robust autoantibody response
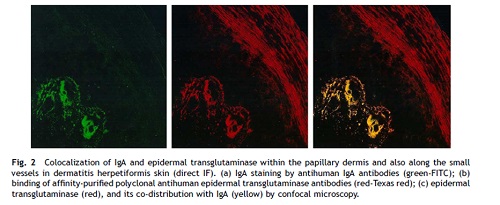
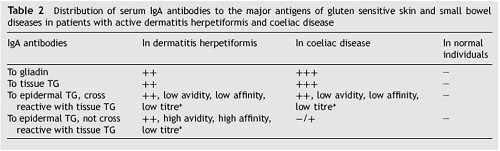
• Circulating IgA and/or IgG anti-tTG and antigliadin antibodies are found in patients with active CD.• However, in patients with DH, eTG appears to be the dominant autoantigen, and it colocalizes with IgA deposits in the skin• eTG is homologous to tTG within the enzymatically active domains
• The pathogenic autoantibodies in both CD and DH are predominantly of the IgA class, although IgG can be seen and becomes important in patients with gluten sensitivity and IgA deficiency
• Although the main autoantigens differ between CD and DH, one study showed that they share common conserved epitopes, further linking the two diseases
• The majority of children with CD have higher levels of anti-tTG than eTG IgA antibodies compared to adults with either CD or DH
• Iodine use and iodine-containing diets (such as shellfish) have been reported to induce flares of DH. Recently, the exacerbation of DH was shown to occur after exposure to triiodomethane containing material used during dental procedures
• Tobacco
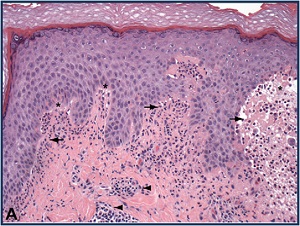
• Because the initial neutrophilic infiltrate in DH is within the dermal papillae, most investigators (supported by em studies ) • immunomapping has confirmed that the subepidermal cleft is, in fact, within the lamina lucida
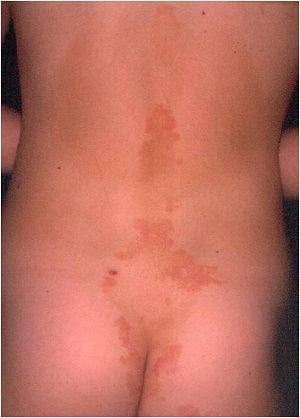
Clinical features• symmetrical distribution on the extensor surfaces of the upper and lower extremities, elbows, knees, scalp, nuchal area, and buttocks
 |
 |
 |
 |
 |
 |
 |
 |
 |

• Severe pruritus, burning, and/or stinging, alone or preceding the eruption by 8 to 12 hour are often the presenting symptoms, simulating scabies. • Localized scalp lesions
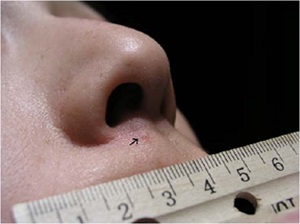
• An uncommon skin manifestation of DH ispalmoplantar purpura. This finding is more common in children, but a number of adult cases have been describedMucosal involvement is rarely seen in DH.• dental abnormalities have been described in patients with CD and in patients with DH

• LABD• bullous pemphigoid
• Urticaria• atopic,nummular or contact dermatitis
• scabies
• enteropathy
• Isolated iron deficiency
• thyroid disease and presence of thyroid microsomal antibodies
• type I diabetes
• Addison disease
• Vitiligo ,alopecia areata, autoimmune connective tissue diseases
• non-Hodgkin lymphoma• increased risk of osteoporosis and fracture
• PE• Histopathology
• DIF (pathognomonic)
• Serology
• Genetic testingBiopsyDermatitis herpetiformis19
specimens for routine histopathology should ideally contain an intact vesicle.
LABDBullous
LE
• Acantolysis of basal keratinocytes
• Normal skin
• secondary changes related to excoriation, or nonspecific
• To avoid this pitfall, one should consider routinelysubmitting portions of the perilesional skin whenperforming a biopsy for the diagnosis of DH.
Dermatitis herpetiformis20• Normal appearing perilesional skin
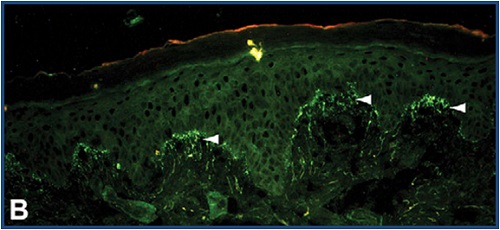
• IgA deposition :linear ,fibrillar
• These cases may clinically differ from classic DH, because some of these patients have had urticarial or psoriasiform lesions.
• use a reputable laboratory
• If there is a strong suspicion for DH and a negative DIF is encountered, serial sections should be taken through the specimen, because this may reveal diagnostic findings
• prolonged GFD ?
• IgA anti-endomysial abs (CD –DH )• IgA-anti TTG specificity :97.6% -100% sensitivity :48.8% to 89.1%. useful in differentiating DH from LABD and reflects the degree of mucosal changes on small bowel biopsy specimens in these patients
• IgA anti-eTG : high sensitivity (60-80.8%) and specificity (92.8- 100%)
• It may become a useful initial screening method in patients in whom DH is suspected clinically• In patients with IgA deficiency, IgG antibodies to endomysium and transglutaminases may be useful to monitor disease
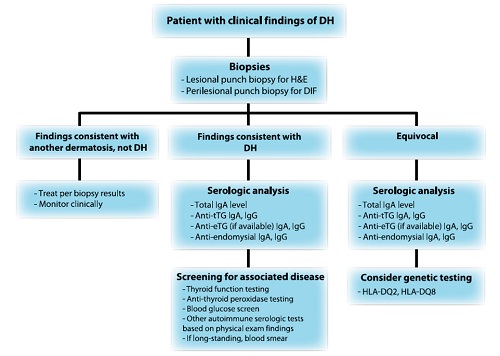
• A biopsy specimen of the small bowelis usually not necessary in DH work-up
• TSH and anti-TPO Ab titer
• FBS• Connective tissue abs
• blood smear
• Family screenings (IgA-TG2 antibody screening )
MANAGEMENT
• gluten-free diet
• strict adherence to a GFD leads to the resolution of skin disease and an improvement in bowel pathology
• Consultation with a dietician is recommended
Gluten free diet• Avoid wheat, barley, and rye• Oat ?
• The advantages of a GFD : relieving the clinical symptoms of gluten sensitivity , decreases the malabsorption , nullify the increased risk of lymphoma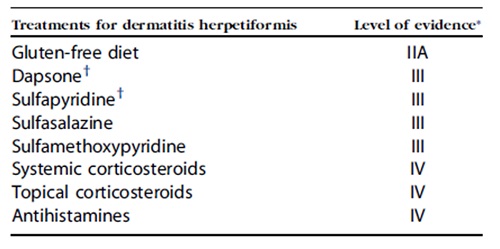
• Dapsone :antiinflammatory and antibacterial properties and inhibits neutrophil recruitment and local neutrophil- and eosinophil mediated tissue injury• 25-100mg/d
• Needs team approach
• Regular visits
• screening of family members
• One study has shown that only 15% of patients adhering to a GFD remained on a steady dose of dapsone, while the remainder were able to stop or reduce the daily dose by 50% or more.
• Overall, 10- and 15-year survival rates in patients with DH do not appear to differ from those of the general population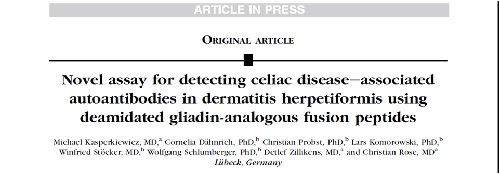
آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
زمان بهترین و ارزشمندترین هدیه ای است كه می توان به كسی ارزانی داشت.هنگامی كه برای كسی وقت می گذاریم، قسمتی از زندگی خود را به او میدهیم كه باز پس گرفته نمی شود . باعث خوشحالی و افتخار من است كه برای عزیزی مثل شما وقت می گذارم و امیدوارم كه با راهنماییهای اساتید این رشته واظهار نظر شما عزیزان این سایت آموزشی پر بارتر گردد.