آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .

• The treatment of melasma includes topical formulations, chemical peels, lasers, and light sources.
• While no single therapy has proven to be of benefit to all patients as the sole therapy, combinations of modalities can be used to optimize management in difficult cases.
SUNSCREENS AND CAMOUFLAGE FOR MELASMA
• Several studies have shown that light from both the ultraviolet (UV) and even the visible spectrum can induce pigmentary changes in the skin, including in Fitzpatrick skin phototypes IV to VI.
• A recent study revealed that visible light can produce significant pigmentation in normal skin, a finding that may be important in the pathogenesis of melasma.
• A broad spectrum UVA- and UVB-protective sunscreen with an SPF of at least 30 along with a physical block, such as titanium dioxide or zinc oxide, should be used by patients with melasma and should be reapplied frequently.
• Patients should also be instructed to wear protective hats and clothing when outdoors and to practice sun avoidance when possible.
• The regular use of broad spectrum sunscreen is effective both in preventing melasma and in enhancing the efficacy of other topical therapies once melasma has developed.
• Broad-spectrum sun protection has been shown to enhance the efficacy of hydroquinone.
• Many patients find the use of camouflage to be an important component in the treatment of melasma.
Topical treatments: The old and the new
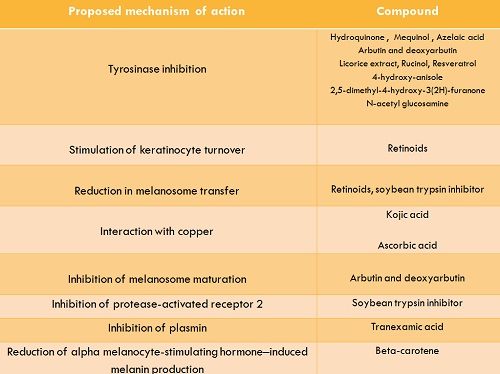
• Because melasma is a disorder of pigmentation, topical treatments are largely aimed at disrupting the enzymatic processes of pigment production within melanocytes.
• Tyrosinase is the rate-limiting enzyme in the process of melanin production, converting L-tyrosinase to L-3,4-dihydroxyphenylalanine (L-DOPA), and is the major target for many of the topical agents. L-DOPA is a required cofactor, and copper is an important molecule that interacts at the enzyme’s active site. Many compounds exhibit multiple effects leading to a decrease in melanization.
PHENOLIC COMPOUNDS
Hydroquinone(1,4 dihydroxybenzene)
• Hydroquinone is thought to act by inhibition of tyrosinase, possibly by binding to the enzyme or by interaction with copper molecules at the enzyme’s active site. This leads to altered melanosome formation and increased melanosome destruction, and perhaps even the inhibition of DNA and RNA synthesis.
• Its efficacy both alone and in combination with other agents is well studied and well established.
• Currently, other agents added to hydroquinone, such as tretinoin and glycolic acid, are responsible for most of the irritation from application of these combination creams.
Over the last several years, concern has been growing over the use of topical hydroquinone preparations:
• Several reports of exogenous ochronosis, a bluish-gray discoloration, have been linked to the use of hydroquinone, especially in South African blacks. In the United States, the occurrence of ochronosis after use of hydroquinone has been much less common.
• One likely explanation for this phenomenon is the fact that hydroquinone can be obtained in higher concentrations (up to 8%) in over the counter formulations in some countries. In addition, these preparations may contain various other ingredients, such as resorcinol, mercury, lemon juice, potash, crushed camphor balls, peroxides, and chlorates that may contribute to the development of exogenous ochronosis.
• One concern regarding hydroquinone is the potential for risks from the production of benzene derivatives after hepatic metabolism. These derivatives are proposed to cause bone marrow toxicity and exert an anti apoptotic effect. However, topically applied hydroquinone bypasses the liver initially, and the major route of metabolism of hydroquinone is via water soluble, renally excreted molecules.
• Another concern is the risk of developing renal adenomas because of potentially toxic metabolites, but topical hydroquinone has not been shown to have renal toxicity.
• In addition, there have been no reports to date of skin or internal organ malignancies occurring in humans as a result of topical hydroquinone application.
• Hydroquinone is commonly found in many foods and beverages, including berries, tea, coffee, red wine, wheat, and the skin of pears.
• Workers involved in the manufacture of hydroquinone have not been found to have any significantly increased risk of premature death or malignancy compared to controls.
• In addition, oral and systemic injections of hydroquinone in animals did not lead to the formation of malignancies or cause marrow toxicity.
• In a review of hydroquinone safety issues, Nordlund et al maintained that there does not appear to be more than a theoretical risk of malignancy and an exceedingly low risk of developing ochronosis or other side effects in patients using available prescription topical preparations of hydroquinone under the supervision of a physician.
Mequinol
• Mequinol (4-hydroxyanisole) is a phenolic agent that is thought to act as a competitive inhibitor of tyrosinase without damaging melanocytes.
• This compound has been approved for use in Europe and USA and is available in combination with topical retinoids.
• Although mequinol has been used as a tyrosinase inhibitor for hyperpigmentation, it has only been studied for lentigines, not melasma. Therefore, a recommendation for melasma cannot be made at this time.
RETINOIDS
• Tretinoin is an effective treatment for melasma but often causes irritation and usually requires months to show improvement as mono therapy may not be very useful as monotherapy for melasma
• The mechanism of action is thought to involve stimulation of keratinocyte turnover, decreasing melanosome transfer and allowing greater penetration of other active ingredients.
• It is thought to inhibit tyrosinase transcription, interrupt melanin synthesis, inhibit tyrosinase related proteins 1 and 2 (TRP-1 and TRP-2), and has been shown to decrease posttranscriptional levels of tyrosinase and TRP-1 after UVB exposure.
• Although tazarotene has been reported to be useful for postinflammatory hyperpigmentation, there have been no published reports of its use in the treatment of melasma.
• Adapalene, a synthetic retinoid with less irritancy, has been tested for the treatment of melasma an tolerate alternative in patients who can not tretinoin
• Although the degree of improvement was modest, adapalene may present a more tolerable and equally efficacious retinoid for use in the long-term treatment of melasma (level of evidence, II-ii).
COMBINATION PRODUCTS
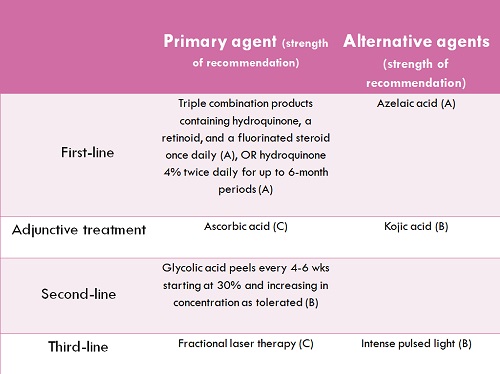
• A combination of hydroquinone, a retinoid, and a topical steroid appears to be highly effective for the treatment of melasma
• One of the first combination topical therapies developed for the treatment of hyperpigmentation was the Kligman-Willis formula, consisting of 5% hydroquinone, 0.1% tretinoin, and 0.1% dexamethasone. The authors found that 10% hydroquinone was more efficacious but more irritating, 0.2% tretinoin was more irritating without being more effective, 0.05% tretinoin was less irritating but required a longer treatment time to see beneficial effects, and dexamethasone could be increased to 0.2% with enhanced activity without much change in irritancy. The researchers also found that fluorinated steroids were more effective than nonfluorinated steroids.
• The time to see benefit with twice daily usage was approximately 3 weeks.
• One theory behind the effectiveness of this combination of agents is that tretinoin prevents the oxidation of hydroquinone and improves epidermal penetration while the topical steroid component reduces irritation from the other two ingredients and decreases cellular metabolism, which inhibits melanin synthesis.
• Since this discovery, other dual and triple agent therapies have been studied. Dual combination topicals tested include hydroquinone plus retinoic acid and hydroquinone plus retinol.
• Concomitant use of regular photoprotection of at least SPF 15 increased the efficacy of topical therapy significantly (level of evidence, II-iii).
• One of the most successful combination formulations has been 4% hydroquinone, 0.05% tretinoin, and 0.01% fluocinolone acetonide. (nightly use)
• Side effects of treatment include erythema, desquamation, burning, dryness, and pruritus;
• Because irritation may lead to the development of postinflammatory hyperpigmentation in patients with darker skin types, a decrease in frequency of application is a reasonable approach to those who develop irritation (level of evidence, I).
• One study confirmed the superiority of this combination cream over hydroquinone alone.
• Another combination that has been tested is 0.05% tretinoin, 0.05% triamcinolone acetonide, 6% hydroquinone, and 0.1% ascorbic acid used nightly with daily photoprotection in an open-label study.
Summary
• Topical therapy with a triple combination agent appears to be the most clinically effective initial therapy for patients with melasma.
• Hydroquinone 4% in conjunction with regular photoprotection, although less effective, is a good alternative to a triple combination agent.
• Retinoids as monotherapy are unlikely to be as efficacious as the above agents and require significantly more time before results are visible.
Some of other commonly topical agents in topical preparations for treatment of hyperpigmentation:
Azelaic acid
• Azelaic acid is a 9-carbon dicarboxylic acid derived from Pityrosporum ovale that acts as a weak reversible competitive inhibitor of tyrosinase.
• This molecule may have cytotoxic and anti-proliferative effects on melanocytes, possibly by interfering with mitochondrial respiration and DNA synthesis in abnormal melanocytes.
• Another possible mechanism of action includes decreased free radical formation.
• The most commonly side effects of preparations containing azelaic acid include pruritus, mild erythema, scaling, and burning.
• It has been shown to be safe for use in combination with retinoids.
• In comparison to hydroquinone, 20% azelaic acid has been shown to have greater efficacy than 2% hydroquinone in a 6-month study and to be equally as efficacious as 4% hydroquinone in a 24-week double blind trial (level of evidence, I).
Kojic acid
• Kojic acid is a molecule produced by Aspergilline oryzae and Penicillium spp.
• It acts as a tyrosinase inhibitor that works by chelating copper at the enzyme’s active site. This agent is usually available over the counter in a 2% concentration.
• It is important to keep in mind that kojic acid is a known sensitizer.
• Studies examining the efficacy of kojic acid in melasma have shown mixed results.
Ascorbic acid
• Ascorbic acid, is thought to decrease pigment by interacting with copper at the active site of tyrosinase and by reducing dopaquinone by blocking dihydrochinindol- 2-carboxyl acid oxidation.
• However, this molecule is rapidly oxidized, highly unstable, and does not work well alone; it is therefore usually combined with licorice extracts and soy to increase efficacy.
• Using iontopheresis with vitamin C in a 12-week randomized double-blind split-face study, Korean women with melasma reported a noticeable improvement on the vitamin C treated side, but there was no long-term follow-up to determine the duration of these effects.
• In another randomized trial, patients who applied 4% hydroquinone cream to one side of the face and 5% ascorbic acid cream to the other noted greater subjective improvement in the hydroquinone-treated side (93% vs. 62.5% on the ascorbic acid site. However, colorimetric analysis showed no difference between treatments.
• Ascorbic acid caused significantly less irritation than hydroquinone; therefore, it may be a useful adjunctive treatment in patients who cannot tolerate hydroquinone because of side effects (level of evidence, I).
Arbutin/deoxyarbutin
• Arbutin is a beta-Dglucopyranoside derivative of hydroquinone that is derived from Uva ursi folium (the bearberry plant) and can also be found in cranberry and blueberry leaves.
• Its mechanism of action is inhibition of tyrosinase and 5,6-hydroxyindole-2-carboxylic acid (DHICA) polymerase and inhibition of melanosome maturation.
• The synthetic deoxyarbutin is a more potent tyrosinase inhibitor and in guinea pig and human tests has been shown to be more effective more rapidly.
• Deoxyarbutin was shown to be as effective in inhibiting mushroom tyrosinase as hydroquinone, and deoxyarbutin-induced skin lightening of solar lentigines was actually maintained without the use of maintenance therapy, whereas hydroquinone-induced skin lightening was not sustained.
• It has been used in Japan at 3% concentrations, but a higher concentration may cause paradoxical hyperpigmentation.
• These agents have not been reported in the treatment of melasma (level of evidence, II-i).
Licorice extract
• Licorice extract inhibits tyrosinase, especially the rate-limiting first step of oxidation. The active ingredients are liquiritin (which disperses melanin) and isoliquiritin (which contains flavonoids).
• It also has topical anti-inflammatory properties.
• A split-face trial treated 20 women with epidermal melasma with liquiritin cream to one half of the face and vehicle cream to the other side twice daily for 4 weeks along with sun avoidance or sunscreen. Sixteen of 20 patients had a clinically graded excellent response (defined as no difference between lesional and normal skin) on the liquiritin-treated side. In contrast, only one patient showed a moderate clinical response on the control-treated side. Patients generally use 1 g per day for 4 weeks before any benefit is seen (level of evidence, II-i).
Soy
• Soybean trypsin inhibitor reversibly inhibits the protease-activated receptor-2 (PAR-2) pathway that is needed for melanosome transfer by keratinocyte phagocytosis of melanosomes.
• In vitro and animal studies show that activation of the PAR-2 pathway enhances melanosome ingestion by keratinocytes, but direct keratinocyte melanocyte contact was required for this to occur. Inhibition of this pathway caused a dose-dependent loss of pigmentation by as early as 4 weeks at the highest tested dose.
• In a multi agent comparative trial in patients with solar lentigines, soy extract was shown to have a modest effect in lightening the lesions.
• However, no trials in melasma patients have been published to date, making it difficult to directly compare the efficacy of soy to other well studied compounds.
Summary
• Azelaic acid may represent a useful second-line topical therapy in patients who do not tolerate or do not have access to preparations containing hydroquinone.
• Ascorbic acid may also be a useful adjunctive topical therapy.
• Kojic acid may give modest improvement for melasma, but it often causes irritation.
• Soy inhibition of the PAR-2 pathway provides a novel approach to treating melasma, but clinical trials are needed to better determine its efficacy.
• Additional studies are needed to determine the role of arbutin/deoxyarbutin and licorice extract in the treatment of patients with melasma.
CHEMICAL PEELS
Alpha hydroxy acid peels
• Glycolic and lactic acids are food-derived alpha hydroxy acids often used in chemical peels for disorders of hyperpigmentation. They are thought to work by inhibiting tyrosinase activity in a pH independent manner.
• These agents have been shown to decrease melanin formation in a dose dependent fashion using melanin assays in mouse B16 and human melanoma cell lines.
Glycolic acid peels
• Glycolic acid peels in increasing concentrations may be a useful adjunct to topical therapy, especially if patients are pretreated with hydroquinone for 2w before the procedure.
• However, given the risk of post procedure hyperpigmentation, a thorough discussion of the risks and potential benefits should be undertaken with the patient before treatment. ( side effects erythema and desquamation, and postinflammatory hyperpigmentation )
Lactic acid peels
• Lactic acid peels have not been studied well enough to recommend their use at this time.
Salicylic acid peels
• Salicylic acid is a beta-hydroxy acid that has been studied as a treatment for melasma and postinflammatory hyperpigmentation resulting from acne
• Salicylic acid peels have not been shown to add any significant benefit to topical therapy in melasma patients and do not appear to be effective as monotherapy
Other chemical peels
• Other agents that have been used for chemical peeling include 1% tretinoin, Jessner solution (composed of salicylic acid, lactic acid, resorcinol, and ethanol), and 10% to 50% TCA peels.
• The addition of chemical peels to depigmenting agents may not add any long-term benefit in patients with melasma (level of evidence, II-i).
Summary
• Glycolic acid may be the most efficacious alpha hydroxyl peeling agent for melasma, but it should be used cautiously.
• Glycolic acid peels should be used in conjunction with a depigmenting agent for maximal benefit and to minimize the risk of postinflammatory hyperpigmentation.
• Salicylic acid peels appear to be of minimal benefit in the treatment of melasma
• Although chemical peels may improve disorders of hyperpigmentation by removing unwanted melanin, they can also cause irritation, which can lead to postinflammatory hyperpigmentation. This side effect is especially common in patients with darker skin types; therefore, peels or any other procedure causing injury to the skin should be performed with extreme caution in patients with melasma.
LASER AND LIGHT THERAPIES
• The use of laser and light therapy for melasma is based on several observations: (1) melanin has a broad absorption spectrum, allowing a variety of lasers and light sources to be used; (2) melanosomes have a short thermal relaxation time, in the range of 50 to 500 nanoseconds; and (3) longer wavelengths penetrate deeper to target dermal pigment, but melanin absorption is better with shorter wavelengths.
• This therapeutic modality is more challenging because damage to surrounding tissue and subsequent inflammation can lead to postinflammatory hyperpigmentation, which may be long lasting and even delayed in onset.
• Therefore, lasers and light-based therapies should be used after other modalities have been proven to be unsuccessful and should be used with extreme caution in Fitzpatrick skin phototypes IV to VI.
• Q-switched ruby lasers has been shown to worsen melasma
• erbium:YAG lasers(emits at 2940 nm and targets water as its chromophore and is therefore useful for ablative resurfacing) has been shown to worsen melasma
• The combination of carbon dioxide laser (targets water as its chromophore and can be helpful in removing epidermal pigmentation) with Q-switched Alexandrite laser (emits at a longer wavelength than some other Q-switched lasers (755 nm) and therefore penetrates deeper into the skin) does not appear to be beneficial for melasma and carries a significant risk of worsening hyperpigmentation in darker-skinned patients
Fractional resurfacing
• Fractional resurfacing is a newer technology that creates microzones of thermal damage.
• It does not cause full-thickness epidermal wounds, so recovery is more rapid and, theoretically, the resulting inflammation and dyspigmentation is less of a risk.
• The microthermal zones of injury limit the area of skin that is damaged with each treatment, which may decrease the risk of postinflammatory hyperpigmentation.
• In addition, the transepidermal elimination of these microthermal treatment zones after injury could serve as an effective method of removing dermal melanophages.
• Fractional laser therapy is the only laser treatment for melasma that has been approved by the FDA, and it has shown promising results.
• Given the risk for hyperpigmentation, some authors suggest using lower fluences, variable pulses, and pretreating all patients with hydroquinone for up to 6 weeks before laser therapy, especially in patients with a history of postinflammatory hyperpigmentation.
• however, additional controlled trials are needed to evaluate its efficacy for melasma.
Intense pulsed light (IPL)
• Intense pulsed light (IPL), a non-laser light source that emits light with wavelengths between 515 and 1200 nm.
• IPL appears to give modest improvement as an adjunctive therapy in patients with melasma refractory to topical therapy alone and may be useful in patients who do not mind the 1- to 2-week recovery time.
Copper bromide laser
• Copper bromide lasers can produce two wavelengths of light that may be emitted separately or together. The 511-nm green beam is used to treat pigmentary lesions, while the 578-nm yellow beam is used to treat vascular lasers.
• Copper bromide lasers may be of benefit for melasma, especially in patients with a visible vascular component, but require further study.
Summary
• Fractional laser therapy appears to be the most promising laser or light treatment for melasma; however, there is still a long-term risk of post procedure hyperpigmentation and a possible need for maintenance therapy.
• IPL treatment may also provide modest benefit as an adjunctive treatment.
• Copper bromide lasers may also be beneficial in a select population of patients, but larger studies are needed before this therapy can be widely recommended.
• Given their cost and the need for multiple treatments, laser and light therapies should be considered third-line treatments in severe refractory patients who have not responded to topical preparations or chemical peels and who are willing to accept the risks of these procedures.
ON THE HORIZON Because no panacea for melasma has yet been found, investigators continue to search for novel inhibitors of melanin synthesis. Several new compounds are being studied as possible treatments of melasma.
Rucinol
• Rucinol, a derivative of resorcinol that inhibits tyrosinase and TRP-1 in a dose-dependent manner in B16 mouse melanoma cells, has been shown in a vehicle-controlled, split-face, doubleblind randomized trial to have a modest effect on epidermal and mixed melasma lesions in patients with Fitzpatrick skin phototypes III to V.
• Interestingly, broad-spectrum sun protection alone used on the control side also showed a significant benefit (level of evidence, I).
Tranexamic acid
• Tranexamic acid is a plasmin inhibitor and lysine analog that has been shown to prevent UV-induced pigmentation in guinea pigs. In keratinocytes, it prevents the binding of plasminogen to keratinocytes, which leads to less free arachidonic acid and subsequent decreased production of prostaglandins. This in turn leads to a decrease in tyrosinase activity in melanocytes.
• Of note, topical tranexamic acid can cause allergy or irritation, so newer liposomal delivery systems have been created to improve tolerability.
• Intradermal tranexamic acid injections have been investigated in 100 patients with Fitzpatrick skin phototypes IV to VI and mixed or dermal melasma. Investigators found that changes in MASI were statistically significant (mean MASI 13.22 at baseline compared to 7.57 after 12 weeks of weekly injections), but clinically significant improvement was not seen until 4 weeks of treatment. No long-term follow-up was performed (level of evidence, II-iii).
Beta-carotene
• Beta-carotene is a structural analogue of vitamin A that decreases melanin production and is under investigation for use in treating disorders of hyperpigmentation.
DMHF (2,5-dimethyl-4- hydroxy-3(2H)-furanone)
• Using B16 melanoma cells, DMHF has been shown to decrease alpha melanocyte-stimulating hormone (a-MSH)e induced melanin content and tyrosinase activity without being cytotoxic. Even more intriguing are the findings that DMHF can inhibit production of microphthalmia- associated transcription factor and tyrosinase, reduce the production of TRP-1 (but not TRP-2), and block a-MSHe induced increases in melanin in normal human melanocytes.
• No published clinical trials are available.
• Based on the current evidence, broad spectrum UV and visible light protection and avoidance and topical depigmenting agents appear to be the most useful therapies for melsma.
• Still unclear if chemical peels or laser and light sources significantly improve these patients, but there have been a few promising developments in the use of procedures for melasma.
آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
زمان بهترین و ارزشمندترین هدیه ای است كه می توان به كسی ارزانی داشت.هنگامی كه برای كسی وقت می گذاریم، قسمتی از زندگی خود را به او میدهیم كه باز پس گرفته نمی شود . باعث خوشحالی و افتخار من است كه برای عزیزی مثل شما وقت می گذارم و امیدوارم كه با راهنماییهای اساتید این رشته واظهار نظر شما عزیزان این سایت آموزشی پر بارتر گردد.