آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
An Evidence-Based Review
Am J Clin Dermatol 2012; 13 (3): 141-152
Introduction
Acne vulgaris is a highly prevalent skin disease and the most common skin disorder in adolescents.
Numerous treatment options are available, but topical antimicrobial therapy remains a mainstay for the management of mild to moderate acne because it offers localized treatment with less risk of systemic adverse effects.
Literature Search
The literature review conducted for this paper includes searches in the following databases:
Ovid
MEDLINE
EMBASE
and the databases of the Cochrane Library.
Concepts searched included acne vulgaris and topical antibiotics.
Terms that describe the concepts include ‘acne vulgaris,’ ‘topical anti-microbial,’ ‘anti-infective agents,’ ‘anti-bacterial agents,’ ‘dermatologic agents,’ ‘benzoyl peroxide,’ ‘sodium sulfacetamide,’ ‘azelaic acid,’ ‘clindamycin,’ and ‘erythromycin.
These terms were searched both as text words and as subject headings.’
All searches were limited to:
controlled trials
systematic reviews
No year limits were applied to the searches and they therefore extend as far back as the year range of each database up to April 2011 when they were conducted.
Retrievals in Ovid MEDLINE go back to 1976
EMBASE to 1985
the Cochrane Library to 1966
Mechanisms of Action of Anti-Acne Agents
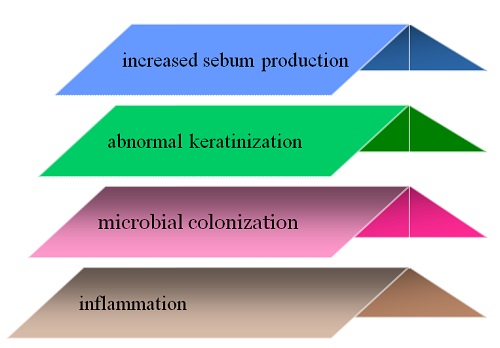
Several factors contribute to development of acne including:
Several factors contribute to development of acne including:
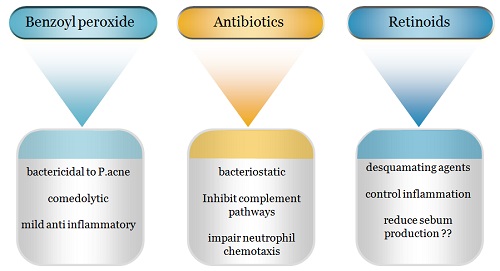
Antibiotics, retinoids, and benzoyl peroxide have complementary mechanisms of action that may contribute to their synergistic activity when used in combination.
Retinoids reducing keratinization.
antibiotics and benzoyl peroxide reducing inflammation and P. Acnes counts.
The desquamating effect of retinoids also increases the penetration of antibiotics.
Interestingly, use of benzoyl peroxide with retinoids may decrease retinoid activity although newer retinoids such as adapalene are more stable and may be used in combination with benzoyl peroxide.
Treatment of acne vulgaris with benzoyl peroxide alone or in combination with other topical treatments at concentrations of 2–5% is the standard of care for mild to moderate papularpustular acne.
Use of benzoyl peroxide 2.5% appears to offer similar benefit to the 5% and 10% concentrations with fewer associated adverse effects.
Benzoyl peroxide monotherapy has been shown to have greater activity than topical tretinoin or isotretinoin against inflammatory lesions, although two smaller trials demonstrated similar efficacy for both agents.
Benzoyl peroxide is available in a variety of preparations including gels, washes, lotions, and creams.
There is no clear superiority of these different preparations in terms of effectiveness.
Topical antibiotics are most effective for treating inflammatory acne, with limited efficacy against non-inflammatory lesions.
The most commonly available antibiotics for topical treatment of acne are erythromycin and clindamycin.
Bacterial resistance is a persistent problem with antibiotics, especially when they are used as monotherapy.
The efficacy of erythromycin, in particular, may be declining due to bacterial resistance.Increasing bacterial resistance has led many experts to recommend against the use of antibiotics as monotherapy.
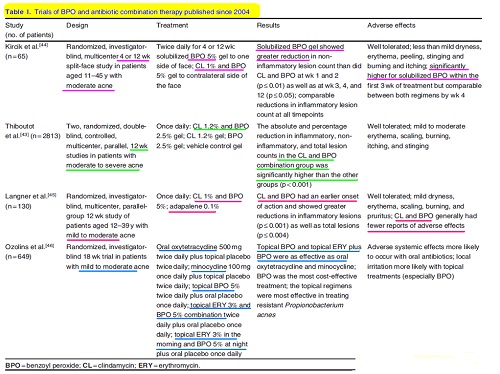
Two large randomized, double-blind, controlled studies from 2008 showed that benzoyl peroxide 2.5% and clindamycin 1.2% gel significantly reduced lesion counts.
A recent meta-analysis determined that combination benzoyl peroxide 2.5%or 5%with clindamycin outperformed benzoyl peroxide and clindamycin monotherapy in treating inflammatory lesions and that reduction of non-inflammatory lesions with benzoyl peroxide 2.5% and clindamycin was significantly greater than any of the other treatments.
A study by another also showed that benzoyl peroxide 2.5%and clindamycin preparation demonstrated similar efficacy to benzoyl peroxide 5% and clindamycin preparation but was better tolerated.
Benzoyl peroxide monotherapy produced similar results to combined erythromycin and benzoyl peroxide treatment in both primary outcome measures, although it produced greater skin irritation than the erythromycin and benzoyl peroxide combination
Several studies have demonstrated that combination therapy with topical retinoids and antibiotics produces significantly faster and greater clearance of acne than topical antibiotics or topical retinoids alone.
The combination of retinoids with antibiotics may be less irritating to the skin compared with monotherapy.
Combining clindamycin with the newer topical retinoids adapalene and tazarotene is more efficacious than clindamycin and tretinoin combination therapy.
Adapalene also causes significantly less skin irritation than tretinoin when used in combination with topical clindamycin.
Unfortunately, these agents are also more costly.
Additional options for topical treatment of acne include:
dapsone
zinc
sodium sulfacetamide
salicylic acid
azelaic acid
allylamines
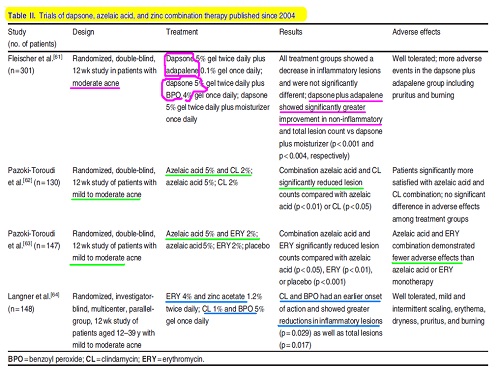
Topical dapsone 5%, alone or in combinationwith adapalene 0.1% or benzoyl peroxide 4%, has been shown to be safe and efficacious, but may be more irritating to the skin than other topical agents.
Topical antibiotics are also available in combination with zinc acetate.
While zinc is ineffective as monotherapy, a small, single-blind study of patients with mild to moderate acne treated with benzoyl peroxide 5% plus clindamycin 1% or erythromycin 4% plus zinc acetate 1.2% once daily found that, although both regimens improved total lesion count, clindamycin plus benzoyl peroxide had an earlier onset of action and showed significantly greater reductions of inflammatory lesions as well as total lesions.
A small observational study demonstrated that 20% sodium sulfacetamide, when used in combination with a 50% sulfur foam, decreases acne, rosacea, and seborrheic dermatitis lesions without adverse effects.
Limited evidence also shows that salicylic acid alone, or in combination with benzoyl peroxide can improve acne. While limited safety data exist, it has been suggested as an alternative for patients who cannot tolerate topical retinoid therapy.
An Iranian trial of patients randomly assigned to combination azelaic acid 5% and clindamycin 2%, or either agent alone, showed that the combination gel significantly reduced total lesion count compared with baseline, as well as clindamycin 2%or azelaic acid 5%monotherapy.
The same group found similar results when combining azelaic acid with erythromycin and noted that the combination was more tolerable than either agent used alone.
Other studies have shown that azelaic acid at concentrations of 15–20% demonstrates efficacy and tolerability comparable to tretinoin, benzoyl peroxide, and erythromycin monotherapy for the treatment of mild to moderate forms of acne.
Combination therapy utilizing benzoyl peroxide in combination with an allylamine (an antifungal agent), demonstrated more effective control of comedones than benzoyl peroxide monotherapy.
Bacterial Resistance
The long-term, low-dose antibiotic regimens often prescribed for acne treatment have been associated with increasing P. acnes resistance.
Macrolides, such as erythromycin, are most associated with the development of bacterial resistance, although resistance to clindamycin, tetracycline, and other antibiotics is also quite high.
A study in the UK found that resistance to erythromycin and clindamycin increased from nearly 35% in 1991 to over 55% in 2000.
A similar study comparing patterns of resistance in several European countries found that resistance to erythromycin and clindamycin may be as high as 90% in some regions.
P. acnes and Staphylococcus epidermidis strains can transfer resistance to Staphylococcus aureus and increase the lethality of that organism.
These findings have prompted scientists to recommend against the use of topical or oral antibiotics as monotherapy for acne vulgaris.
Benzoyl peroxide appears to be effective in controlling both antibiotic-sensitive and antibiotic-resistant P. acnes.
Use of combined agents may allow for reduced dosages of antibiotics and lessen selection pressure for resistance.
Use of benzoyl peroxide may also help slow the spread of antibiotic resistant S. epidermidis strains, which are associated with resistance in S. aureus.
One expert panel recommends that if antibiotics must be used for longer than 2 months, benzoyl peroxide should be utilized for at least 5–7 days between antibiotic courses to avoid resistance.
Combination treatment with different types of oral and topical antibiotics should be avoided.
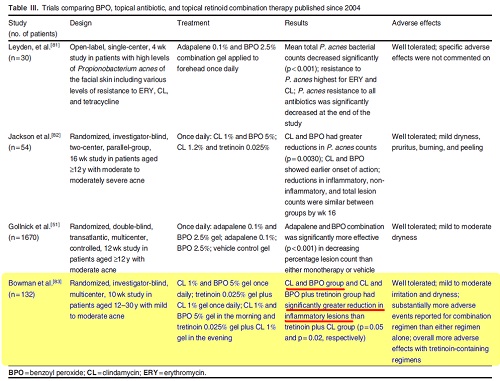
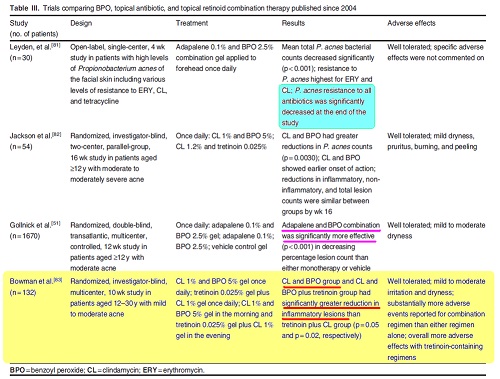
A small open-label study evaluated the effectiveness of combination adapalene 0.1% and benzoyl peroxide 2.5% in reducing antibiotic-sensitive and resistant strains of P. acnes on the facial skin of study subjects. All subjects had strains sensitive and resistant to erythromycin, clindamycin, and tetracyclines at baseline. Mean counts of erythromycin-, clindamycin-, and tetracycline-resistant P. acnes were significantly decreased by week 4 .
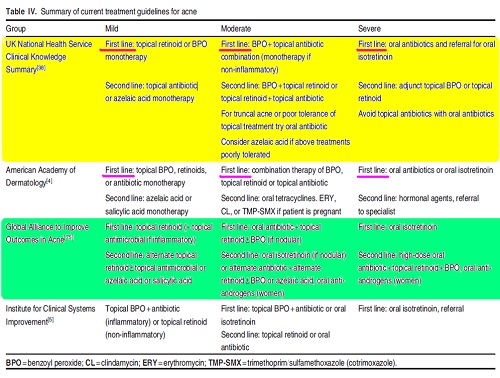
Treatment Selection
Expert Guidelines
Comparing Combination Therapies
Adverse Effects
Cost
Practical Considerations
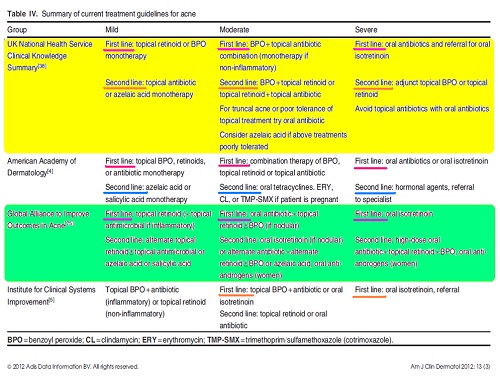
Comparing Combination Therapies
clindamycin 1.2%and tretinoin 0.025%gel
clindamycin 1%and benzoyl peroxide 5% gel.
clindamycin and benzoyl peroxide combination group had a faster reduction in inflammatory and total lesion counts compared with the tretinoin combination group
reduction in inflammatory, non-inflammatory, and total acne lesions were similar by the end of the 16-week study
Reductions in clindamycin-resistant P. acnes colonization occurred only in the benzoyl peroxide group
A randomized, double-blind study conducted in 2003 compared
benzoyl peroxide 5% and erythromycin 3%
tretinoin 0.025% and erythromycin 4% topical gels
1. The number of papules, pustules, and comedones was reduced in the two treatment groups at week 12, with no significant differences between groups
2. The benzoyl peroxide and erythromycin group also demonstrated significantly less erythema and scaling
The authors concluded that for moderate acne vulgaris, benzoyl peroxide and erythromycin may provide a greater beneficial effect than tretinoin and erythromycin.
benzoyl peroxide 5% and clindamycin 1%
adapalene 0.1%
The clindamycin and benzoyl peroxide group exhibited earlier onset of action with significantly greater reductions in total lesions and inflammatory lesions than the adapalene group
Adverse Effects
Localized adverse effects including:
erythema
desquamation
Itching
burning
Where irritation persists, a change in preparation to washes, gels, moisturizing creams, or lotions may help.
Water-based preparations of benzoyl peroxide may cause less skin irritation than the alcohol-based solutions.
benzoyl peroxide has any relationship to the development of skin cancer in humans
While considered safe for use by pregnant women, benzoyl peroxide is categorized within category C by the US FDA
Erythromycin and clindamycin fall within pregnancy category B
Pseudomembranous colitis has been reported with topical clindamycin use
Patients and their parents should be made aware that benzoyl peroxide can
bleach clothing, towels, bed linens, and perhaps even hair.
Cost
Providers and patients must also weigh costs and drug availability in choosing a treatment regimen.
The average total cost of treatment per episode across all age groups is $US689.06.
Topical retinoids are in general more expensive than generic benzoyl peroxide preparations.
Erythromycin and benzoyl peroxide administered separately were nearly three times more cost effective than the proprietary fixed-dose combination.
Practical Considerations
generic preparations more cost effective
combination products convenience and faster speed of onset
Higher concentrations of erythromycin require refrigeration,thus dermatologists sometimes prefer the fixed-dose combination of benzoyl peroxide 5% and clindamycin 1%.
Should consider local patterns of resistance
select the shortest feasible treatment duration
Data indicate that 6–8 weeks is an appropriate timepoint to assess response to antibiotic treatment.
Fails to respond to topical treatments :
Adequate adherence
increasing the drug strength and or frequency of application
combining different topical products
starting an oral therapy.
Poor adherence
reducing the strength of treatment
using a different preparation of the drug
switching to an alternative topical agent that causes less irritation.
آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
زمان بهترین و ارزشمندترین هدیه ای است كه می توان به كسی ارزانی داشت.هنگامی كه برای كسی وقت می گذاریم، قسمتی از زندگی خود را به او میدهیم كه باز پس گرفته نمی شود . باعث خوشحالی و افتخار من است كه برای عزیزی مثل شما وقت می گذارم و امیدوارم كه با راهنماییهای اساتید این رشته واظهار نظر شما عزیزان این سایت آموزشی پر بارتر گردد.