آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
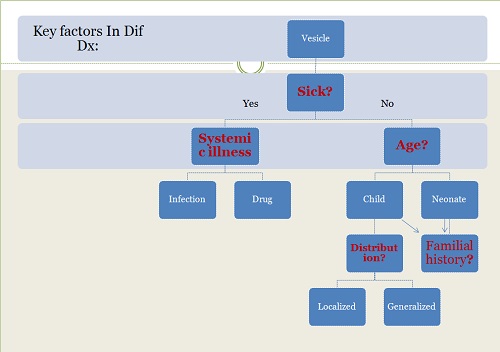
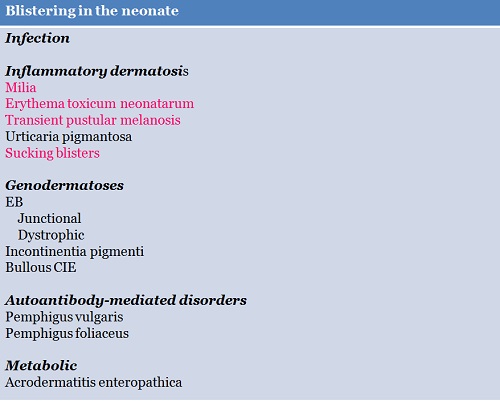
Establishing the correct diagnosis in newborns presenting with blisters and erosions is not always a straightforward process.
Many different disease entities including acquired (i.e., infectious, immunobullous, traumatic) and inherited disorders have to be taken into consideration.
Similarities in clinical appearance, colonization and/or super infections of preexisting skin lesions
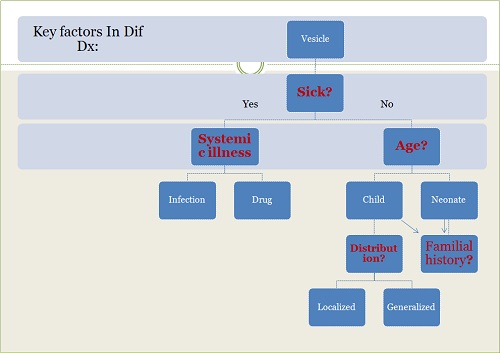
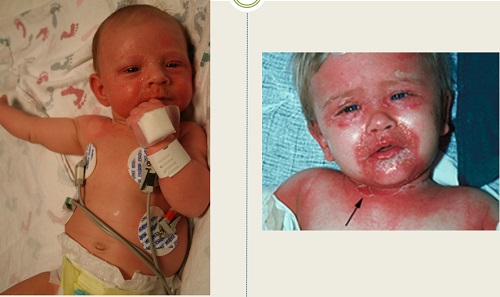
Question?
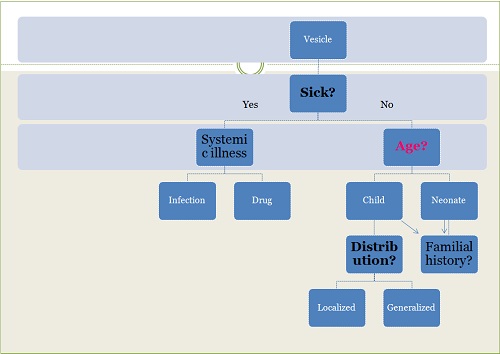
What’s the first decision point in evaluating a child with blisters?
FH
Health status
Time
Localized/generalized
The morphology of lesions(intraepidermal/subepidermal)
Presence of secondary changes
Pattern of eruption( annular, serpiginous or grouped)
Viral
Herpes( H. simplex, H. varicella-zoster), cytomegalovirus, EBV, coxackievirus, poxvirus( varola, monkeypox)
Fungal
Candidiasis ( neonatal cutaneous versus congenital)
Bacterial
a)Gram-positive organisms
Treponema pallidum
Staphylococcus( impetigo neonatarum, SSSS)
Streptococcus( particularly group β-hemolytic)
Bacillus anthracis
b)Gram- negative organisms
E.Coli
H.Influenza
K.Pneumoniae
Infestation
Sarcoptes scabeii
Fever, lethargy, decreased appetite or behavior changes are important signs and symptoms of infection in children
However these finding may be absent in neonate with sepsis
While impetigo neonatarum, neonatal cutaneous candidiasis, thrush and scabies are usually not life-threatening , the remainder of the above condition have the potential of causing devastating infection in the neonate and must be appropriately diagnosed and treated.
Infants & children with normal immune responses are less susceptible to many of the above organisms.
However, they are candidates for impetigo,SSSS and bullous cellulitis due to streptococcus or Haemophilus as well as mucocutaneous candidiasis and herpetic infections.
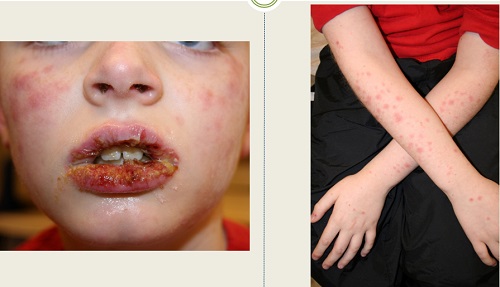
What’s your diagnosis?








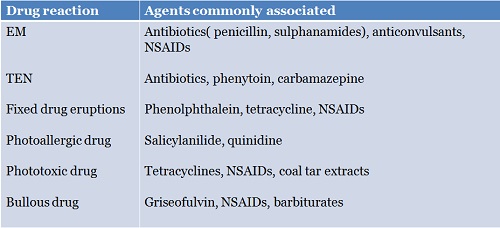
Vesiculobullous adverse reaction to drugs
Q & Tips…
What’s the most common agents associated with adverse reactions in children ?
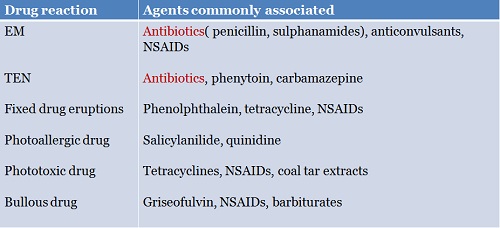
Vesiculobullous adverse reaction to drugs
What’s your diagnosis?


Tips….
Blisters which are present at birth or within the first 72 h may arise as a consequence of an:
Inflammatory cutaneous process
Congenital infection
Genodermatosis or rarely
Transient autoimmune blistering diseases
What’s your diagnosis?





Familal history
Is important particularly in evaluating neonates with blister
Dif dX for blister at birth or in the immediate postpartum period:
Genodermatosis/Mechano-bullous
Transient autoimmune blistering diseases
In patients with autosomal recessive defects such as RDEB or in whom a spontanous mutation , familial history may e non-contributory
Junctional and dystrophic EB often present at birth or shortly after with bullae and erosions typically by passage through the birth canal.
Presence of scarring and milia indicates that intra uterine blistering has occurred.
Disorders associated with FH of blistering
Autoantibody-mediated disorders
As pemphigus vulgaris is uncommon in young or middle aged women, neonatal pemphigus vulgaris is also uncommon.
23 cases of neonatal pemphigus have been reported since then, the first in 1975
Of the 23 cases 20 mothers had PV, two cases had pemphigus foliaceus, one had pemphigus vegetans.
About PV: including women in remission
Antibody titer of mother or newborn or clinical presentation of mother at the time of delivery do not predict the severity of neonatal PV.
There are reports of neonatal PV in newborns from mothers with no active disease and cases of non affected neonates born from mothers with highly active disease
46 cases of PV
Till date, 29 cases of sporadic PF in children have been reported
Cases under 10 years of age are extremely rare implying an increase in incidence during puberty
Generalized blistering disorders
What’s the most common cause of generalized vesicle in an infant or child ?
Localized blistering disorders
Approach to the child with vesiculo bullous lesions
آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
زمان بهترین و ارزشمندترین هدیه ای است كه می توان به كسی ارزانی داشت.هنگامی كه برای كسی وقت می گذاریم، قسمتی از زندگی خود را به او میدهیم كه باز پس گرفته نمی شود . باعث خوشحالی و افتخار من است كه برای عزیزی مثل شما وقت می گذارم و امیدوارم كه با راهنماییهای اساتید این رشته واظهار نظر شما عزیزان این سایت آموزشی پر بارتر گردد.