آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
Basic principles of cutaneous photobiology
The nature of UVR
• Cutaneous photobiology is the study of the effects of UV and visible radiation on skin.
• Knowledge of the interaction of sunlight with the skin is fundamental to understanding the pathogenesis of more than 100 skin disorders and also skin cancers.
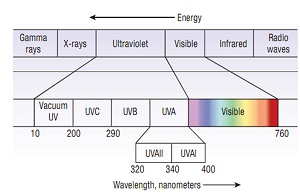
• The UVR spectrum comprises three wavebands:
UVC (100–280 nm)
UVB (280–320nm )
UVA (320–400 nm )
• visible light : 400–700 nm
• UVA has been subdivided into UVA-I (340–400 nm) and UVA-II (320–340 nm) because, the effects of UVA-II are more like those of UVB .
Electromagnetic spectrum:
(The shortest wavelengths are associated with the highest energy and the longest wavelengths with the lowest energy radiation)
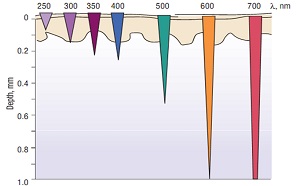
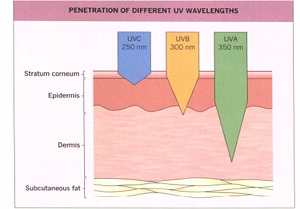
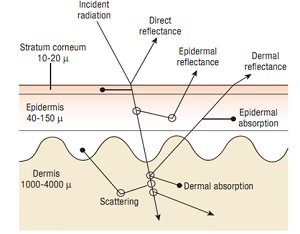
Within the skin, the depth of penetration of UV light is wavelength dependent, the longer the wavelength, the deeper the penetration.
• UVA readily reaches the dermis, most of the UVB is absorbed in the epidermis, and only a small proportion reaches the upper dermis. UVC, if it reached the earth's surface, would be absorbed or reflected predominantly in the stratum corneum and in upper layers of the epidermis.
Sources of UVR
• The sun and other stars :
Practically all of the UVC, and much of the UVB, are absorbed by the oxygen and ozone in the earth's atmosphere, so that UV radiation below 290 nm is virtually undetectable at ground level .
At noon, the UVB content is 5% and UVA accounts for the remaining 95%. When the sun is lower, early or late in the day, the UVA content is even higher.
• Artificial source:
mercury or xenon lamps, UVB or UVA fluorescent tubes, commonly used for phototherapy or cutaneous phototesting. fluorescent tubes, quartz halogen lamps used for room lighting, emit moderate amounts of UVA but minimal UVB
UVR interaction with skin
• 5% of the UVR incident on skin is diffusely reflected, the remainder being transmitted, scattered and absorbed,or passed out of the medium.
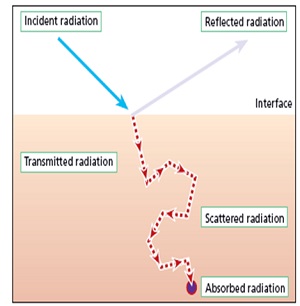
• The UVR absorbing molecule, known as the chromophore.
After absorption ,it contains extra energy and may be altered to form a new molecule called a photoproduct that initiate responses in skin cells so absorption is the first step for photochemical reactions.
• Biomolecules that absorb in the UVB spectrum are:Purine and Pyrimidine bases in DNA and RNA,Urocanic acid,aromatic amino acids in proteins and 7dehydrocholestrol.
• Biomolecules that absorb in the UVA spectrum are: Nicotinamide dinucleotide phosphate,hemoglobin,bilirubin and B carotene.
• Melanin absorb throughout the UV spectrum without a distinct absorbtion maximum wavelength.
• Different wavelengths of UV light induce different types of DNA damages. UVC and UVB, but much less so UVA, are capable of exciting the DNA molecule directly and subsequently generate DNA photoproducts.
• Indeed, DNA is regarded as the chromophore for most of
the biologic effects of UVB and UVC, including erythema, tanning,immunosuppression, mutagenesis and carcinogenesis.
• DNA photoproducts are dimers, formed by covalently binding two adjacent pyrimidines in the same polynucleotide chain. The two major types of pyrimidine dimers are cyclobutane dimers (CPD) and 6,4-photoproducts.
• The absorption maximum of DNA is at 260 nm. This makes UVC the most effective wavelength for the induction of DNA photoproducts in naked DNA. However, due to the absorption of shorter wavelengths in upper layers of the epidermis, 300 nm (UVB) is the most effective wavelength for inducing DNA photoproducts in the basal layer of the epidermis.
• It has recently been shown that UVA can also generate pyrimidine dimers, albeit at a lower frequency than UVB.
• Of note, many of the biologic properties of UVA, including its toxicity to cells, are strictly dependent upon the presence of molecular oxygen, which points to a prominent role for reactive oxygen species.
• Although these reactive oxygen species are also formed by UVB, UVA has been shown to be responsible for almost all oxidative DNA damage after exposure of cells to natural sunlight.
• UVA Pyrimidine Dimer(type I photosensitivity)
• UVA reactive oxygen species(type II photosensitivity)
• UVB Pyrimidine Dimer
• UVB reactive oxygen species
• Photosensitivity responses are usually mediated by reactive oxygen species(ROS).
• Oxygen species react predominantly with guanine and generate several DNA changes, including the mutagenic 7,8-dihydro8-oxoguanosine.
• The oxidative stress affects not only DNA, but also membranes and proteins.
Repair of UV-Induced DNA Damage
Pyrimidine dimmer nucleotide excision repair (NER)
• NER involves recognition of DNA damage, incision of the DNA strand containing a lesion, and DNA synthesis and ligation to replace an excised oligonucleotide.
Oxidative DNA damage base excision repair(BER)
Normal cutaneous effects of UVR exposure
• Acute and subacute effects :
acute inflammatory erythema (sunburn),Immediate tanning( pigment darkening), delayed tanning, epidermal hyperplasia, immunologic changes and
vitamin D3 synthesis
• Chronic effects:
photoaging and photocarcinogenesis
• acute inflammatory erythema (sunburn)
UVR absorption by skin leads to epidermal and dermal cellular damage, which is associated with classic signs of inflammation (e.g.,redness,warmth,pain and swelling)
• The action spectra for erythema and CPD formation are similar,that shows DNA is a major chromophore for erythema.
• DNA is damaged both through direct UVB absorption and also secondary UVA-induced photosensitization reactions.
• Wavelengths around 300 nm are the most DNA damaging and erythemogenic.
• Following DNA damage ,nuclear transcription factors and cytokine are are induced leading to increased production of serum and epidermal interleukins ,with consequent cellular adhesion molecule activation, mild neutrophil and moderate mononuclear cell infiltration production.
• The typical bright red sunburn develops beginning within 30 minutes to 8 hours, peaking at 12 to 24 hours and diminishing over hours to days in the case of UVB exposure.
• With UVC, the response is pinker in color and shorter in duration, starting within hours, peaking at 5 to 8 hours and fading over hours to a day or so.
• With UVA, the reaction is deeper red in color, is usually more persistent, and often begins during irradiation, before fading over hours to days.
• In a few individuals, brief immediate erythema occurs within seconds of UVR exposure and lasts for minutes.
• After excessive exposure, edema and blistering may occur, which, if widespread, may lead to associated systemic symptoms such as chills and malaise. Such reactions are generally followed by pruritus and desquamation over a period of days to weeks.
• The lowest dose to induce erythema is known as the minimal erythema dose (MED).
• MED is differnt according to Fitzpatric skin phototype and wavelength .
• In individuals with Fitzpatrick skin type I is about 100 Jlm2 for UVC , 300 J/m2 for broad-band UVB and 300 kJ/m2 for broadband UVA .
Tanning:
• Melanin composition of skin is a mixture of pheomelanin and eumelanin.Skin types that tan well have more eumelanin.
Immediate :
Immediate, often greyish, tanning of irradiated skin, may occur within seconds of exposure to 20–120 kJ/m2 of UVA, and short-wavelength visible radiation.
This results from photo-oxidation of existing melanins and redistribution of epidermal melanocytic melanin from perinuclear position into the pripheral dendrities.
.
• The biologic function of immediate tanning is not known and sunburning sensitivity is not apparently decreased .
Delayed tanning:
Also known as melanogenesis,is primarily a UVB response that results from increased activity and numbers of melanocytes.
• Gradually appears over hours to days after cutaneous exposure to 400 J/m2 of broad-band UVB (greater than the MED,particularly in fair skinned subjects), 150–200 kJ/m2 of broadband UVA (somewhat less than the MED) or 100 J/m2 of UVC(about equal to the MED).
• The action spectrum for delayed tanning is similar to that for erythema .
• Delayed tanning is maximal from 10 days to 3-4 weaks depending on UV dose.
• Sunburning sensitivity in white skin is moderately decreased by about two- to four-fold .
Hyperplasia:
• persisting for a month or two, develops over hours to days following UVB or UVC (but generally not UVA) exposure.
• The epidermis and dermis, particularly the inert stratum corneum, thicken giving some protection against subsequent UVR-induced inflammation particulary in the fair skinned people.
Immunological changes:
• UVB, UVC, and, to some extent, UVA irradiation alters epidermal Langerhans cell function, generates suppressor T lymphocytes, and changes the cutaneous cytokine profile.
• A sunburn exemplifies the effect that UV light has on the skin's immune function, in this case a proinflammatory effect.
• On the other hand, UV light clearly has anti-inflammatory/
immunosuppressive properties as well, exemplified by the efficacy of UV phototherapy in the treatment of inflammatory skin disorders.
Mediating proinflammatory/immune-stimulating effects
• Release of proinflammatory mediators by skin cells (e.g. serotonin, prostaglandins, IL-1, IL-6, IL-8, TNF-a)
• Induction of antimicrobial peptides (hypothesized to explain why UV-irradiated skin is not prone to bacterial infections)
Mediating anti-inflammatory/immunosuppressive effects
• Depletion of Langerhans cells or modulation of their antigen-presenting function
• Release of anti-inflammatory mediators by skin cells (e.g. IL-1 0, a-MSH)
• Induction of regulatory T cells (antigen-specific)
• However, it is unlikely that there is a simple threshold between the UV doses that have proinflammatory and those that have anti-inflammatory effects.
• Proinflammatory, anti-inflammatory changes occur side-by-side within different arms of cellular and humoral immune reaction cascades, with varying dose-responses as well as modulation by wavelengths and many individual factors far beyond just the degree of skin pigmentation (skin types)
• An example of individual factors would be the observation that the majority of patients wit psoriasis improve with UV phototherapy, but a small minority flares.
• UV light-induced effects on the immune system involve not only the areas of skin directly exposed to UV light, but also non-irradiated sites.
• This effect mediated by the release of immunosuppressive cytokines such as interleukin (IL)-10 and then ultimately by UV-induced regulatory T cells.
• Recent studies suggest that whereas UVR suppresses adaptive immune responses, such as CHS, it may induce the innate immune response by stimulating the production of antimicrobial peptides in human skin.
Other changes :
• On occasion, otherwise healthy individuals develop photo-onycholysis and increased skin fragility with blistering (pseudoporphyria) following intense exposure to sunlight or tanning beds.
• This may be due to photosensitization by normal levels of endogenous substances such as porphyrins.
• photo-onycholysis and pseudoporphyria are probably UVA-induced .
• The mechanisim is similar to those operating in drug or porphyria-associated photo-onycholysis.
• Mid-dermal elastolysis is characterized by patches of finely wrinkled skin and the loss of elastic fibers in the mid-reticular dermis. its onset is frequently associated with intense UVR exposure.
• Brachioradial pruritus, characterized by primary pruritus of the outer arm, is associated with cervical radiculopathy; however, in many patients, UVR may act as a trigger of the symptoms.
Vitamin D synthesis(Acute systemic effects):
• UVB radiation converts epidermal 7 dehydrocholesterol (provitamin D3) into previtamin D3.
• Vitamin D synthesis is maximal at suberythemogenic doses.
Feel-good and health factors
• Solar radiation is essential the provision of humanwell-being, offering warmth and light, but the UV component of such radiation does not appear to be necessary, apart from vitamin D synthesis.
• A cleavage product of POMC is β-endorphin, an opioid peptide with mood-altering properties . One small study has shown that the opioid antagonist naltrexone could induce withdrawal symptoms in 50% of frequent tanners but not in any infrequent control tanners.
Late effects
Photoageing
• gradual deterioration of cutaneous structure
and function following long-term recurrent exposure to sunlight or artificial UVR sources.
• It is characterized by a chronic inflammatory response to UV light
• The epidermis and dermis are both affected, probably by UVB, but the dermis may be affected to some extent by UVA.
• wrinkling, dryness, coarseness, telangiectasia, yellowness,mottled pigmentation, laxity, loss of tensile strength and comedones are characteristic.
• wrinkling, is due to a loss of collagen fibers and deposits of abnormal degenerative elastotic material within the dermis (actinic elastosis).
• These changes are thought to be mediated by inflammation, with subsequent upregulation of extracellular matrix-degrading proteases and down-regulation of collagen synthesis.
• Recent studies suggest that DNA photodamage, the CPD in particular, may be the trigger for matrix metalloproteinases(MMP)induction which degrade collagen.
• It is not just due to infalamation but also UV-induced mitochondrial mutations which lead to loss of cellular functions that makes wrinkles somehow irreversible.
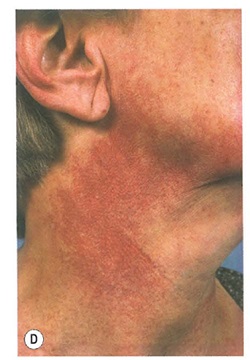
• Photoaging in fair-skinned patients:
Characteristic clinical manifestations are:
Solar elastosis : thickening as well as yellow discoloration of skin that is often in association with marked wrinkling and most commonly seen on the face.
Similar changes occur on the posterior neck and are referred to as cutis rhomboidalis nuchae , characterized by deep skin wrinlding and furrowing associated with a leathery texture.
• solar lentigo: is a light brown to dark brown, even-colored or reticulated macule that are more often multiple. The dorsal aspects of the hands, extensor forearms, upper trunk and face are the most commonly affected sites .
• An ephelide, also known as a freckle, presents as a light brown to medium brown macule, usually less than 6 mm in diameter. Such lesions occur primarily on exposed areas of the face, but also on the shoulders and outer aspects of the arms. Numerous lesions are usually present.
• Poikiloderma of Civatte: refers to reticulated red to red-brown patches with telangiectasias that spare perifollicular skin. It is most commonly observed on the lateral aspects of the neck. there is sparing of the central submental region.
• Mild atrophy and hyperpigmentation are sometimes present.
• Favre-Racouchot syndrome:
• multiple large open comedones develop on the lateral and inferior aspects of the periorbital area in association with marked solar elastosis of the surrounding skin.

• Colloid milium :
characterized by translucent yellow papules that measure 1-3 mm in diameter. There are usually numerous, especially in the neck, face and dorsal hands.

• Erosive pustular dermatosis: classically presents as sterile pustules, crusts, erosions and mild inflammation arising within the photodamaged skin of a bald scalp.
• However, similar clinical findings can occur on the lower extremities of patients with venous hypertension and atrophic skinand following perinatal scalp injuries.

• Photoaging in patients with skin of color
Photoaging is much less pronounced and has a delayed onset in individuals with more darldy pigmented skin. Small seborrheic keratoses, melasma and mottled hyperpigmentation are common signs of photoaging.
• aAny wrinldes are fine and do not appear before 50 years of age.
• Restriction of UVR exposure and the use of high-SPF broad-spectrum sunscreensmay slow progression of this process, and long-term use of the topical retinoid all-trans retinoic acid, and to a lesser extent f α-hydroxyacid preparations, may improve any changes already present
Photocarcinogenesis
chronic cutaneous UVB and, to a lesser extent, UVA exposure are responsible for the induction of most non-melanoma skin cancers, and probably of melanomas as well, although UVA may play a relatively more important part in the latter.
• Because natural sunlight contains much more UVA than UVB and UVA is less filtered by window glass or clothing ,we can say that UVA has a relative contribution to the chronic effect of sun exposure.
• The three major steps of photocarcinogenesis are:
• DNA damage formation after UV exposure
• mutation formation following DNA damage formation
• malignant transformation following mutation formation
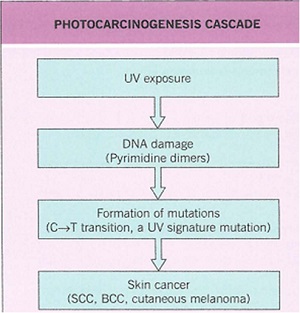
• A number of UVR-induced cutaneous events appear to
be important, including characteristic mutations (C → T andCC → TT) of the p53 tumour suppressor gene in actinic keratoses,squamous cell carcinoma, and basal cell carcinoma and the PTCH gene in basal cell carcinoma .
• A recent study has reported the presence of UVR-induced mutations in the PTEN (phosphatase and tensin homologue) tumour suppressor gene in melanomas in xeroderma pigmentosum (XP) patients
• In the case of photocarcinogenesis, UV exposure not only does it generate DNA damage that leads to mutation formation and malignant transformation, but its immunosuppressive properties:
• The induction of specific tolerance to antigens from UV-induced skin tumors
• reducing the ability of the host immune-defense system to recognize and remove malignant cells.
• impairing immune surveillance against cells
infected with oncogenic viruses (e.g. certain HPV types) and may thereby further promote skin cancer formation.
• Any shift in the balance between pro- and anti-inflammatory responses toward a more immunosuppressed state increases the risk of UV-induced tumor formation, as occurs in chronically immunosuppressed patients.
• Tilting this balance toward proinflammatory responses and autoimmunity increases the risk of developing photodermatoses or photoaggravated skin diseases such as lupus erythematosus.
Suggestive of proinflammatory/immune-stimulating effects
• Sunburn
• Dermatoheliosis
• Photodermatoses (phototoxic and photoallergic)
• Photoaggravation of inflammatory skin diseases (e.g. psoriasis, atopic dermatitis, pityriasis rubra pilaris)
• Induction of autoimmune connective tissue diseases (e.g. cutaneous lupus erythematosus (LE), flares of systemic LE)
• Efficacy of UV phototherapy for the treatment of skin infections (e.g. lupus vulgaris)
• Activation of recurrent orolabial herpes simplex
• Increased risk of photocarcinogenesis in the setting of immunosuppression
(e.g. solid organ transplant recipients)
• Efficacy of UV phototherapy for the treatment of inflammatory skin diseases
• photocarcinogenesis anti-inflammatory effects of UV light
• photoaging chronic inflammatory response to UV light.
• As photocarcinogenesis commonly occurs in photoaged skin, this demonstrates the simultaneous occurrence of pro- and anti-
inflammatory responses to UV light.
Skin phototype Characteristics
I :Always burns, never tans
II : Usually burns, sometimes tans
III:Sometimes burns, usually tans
IV:Never burns, always tans
V :Moderate constitutive pigmentation
VI :Marked constitutive pigmentation
Twisty puzzle solving offers an entertaining way of improving your dexterity and problem solving skills.
آقاي ساسان سلام
اگر بيماري در حال پيشرفت باشد،نقاط جديد بدن كه تازه دارند رنگدانه از دست مي دهند ولي هنوز روند پيشرفت ادامه دارد،خيلي سفيد نيستند،در خصوص سوال دوم،چنين آمپول و درماني وجود ندارد،بهترين درمان براي شما نور درماني هست .
زمان بهترین و ارزشمندترین هدیه ای است كه می توان به كسی ارزانی داشت.هنگامی كه برای كسی وقت می گذاریم، قسمتی از زندگی خود را به او میدهیم كه باز پس گرفته نمی شود . باعث خوشحالی و افتخار من است كه برای عزیزی مثل شما وقت می گذارم و امیدوارم كه با راهنماییهای اساتید این رشته واظهار نظر شما عزیزان این سایت آموزشی پر بارتر گردد.